Not everyone with narcolepsy experiences the same symptoms. Some experience them regularly, while others are less frequently affected.
Symptoms may develop slowly over a number of years, or suddenly over the course of a few weeks.
Narcolepsy is usually a long-term (chronic) condition, although some of the symptoms may improve as you get older.
You should make an appointment to see your GP if you think you may have narcolepsy so they can determine what’s causing your symptoms. If necessary, you’ll be referred to a sleep disorder specialist, who can confirm the diagnosis.
Read more about diagnosing narcolepsy.
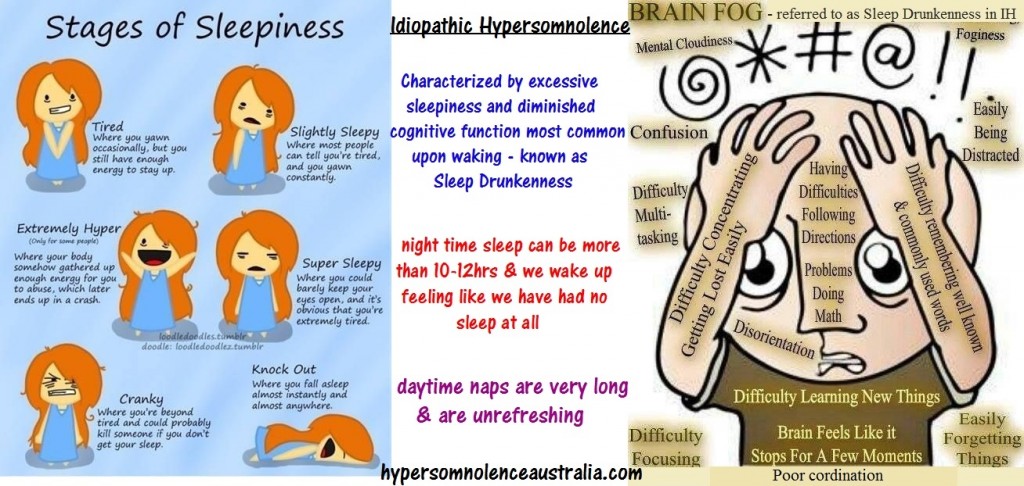
Excessive daytime sleepiness
In most cases, excessive daytime sleepiness is the first sign of narcolepsy. This can have a significant impact on everyday life.
Feeling drowsy throughout the day and struggling to stay awake makes it difficult to concentrate at work or school. People with narcolepsy may be misjudged as being lazy or rude.
Sleep attacks
Sleep attacks – falling asleep suddenly and without warning – are also common in people with narcolepsy. They may occur at any time.
The length of time a sleep attack lasts will vary from person to person. Some people will only have “microsleeps” lasting a few seconds, whereas others may fall asleep for several minutes.
If narcolepsy isn’t well controlled, sleep attacks may happen several times a day.
Cataplexy
Most people who have narcolepsy also experience cataplexy – sudden, temporary muscle weakness or loss of muscular control.
Typical symptoms are:
the jaw dropping
the head slumping down
legs collapsing uncontrollably
slurred speech
double vision or finding it difficult to focus
Cataplexy attacks are usually triggered by an emotion, such as excitement, laughter, anger or surprise. Attacks can last from a few seconds to several minutes.
Some people with narcolepsy have cataplexy attacks once or twice a year, while others experience them several times a day. In an attempt to avoid attacks, some people may become emotionally withdrawn and socially isolated.
Sleep paralysis
Some people with narcolepsy experience episodes of sleep paralysis. This is a temporary inability to move or speak that occurs when waking up or falling asleep.
The episodes can last from a few seconds to several minutes. Although sleep paralysis doesn’t cause any harm, being unable to move can be frightening.
Other symptoms
As well as the symptoms described above, narcolepsy can cause a number of other symptoms, including:
hallucinations – seeing or hearing things that aren’t real, particularly when going to sleep or waking up; a presence in the bedroom is the most commonly reported hallucination
memory problems
restless sleep – for example, having hot flushes, waking up frequently, having vivid nightmares, or physically acting out dreams
automatic behaviour – continuing with an activity without having any recollection of it afterwards
Speak to your GP if you have narcolepsy and it’s making you feel low or depressed.
To find out more please watch the video below!