Introduction
‘Hypersomnia‘ means excessive sleep or sleepiness that interferes with everyday life.
It can have many possible causes, including conditions such as narcolepsy, sleep apnoea or restless legs syndrome; severe sleep deprivation; depression; certain medications (such as tranquillisers); or drug and alcohol misuse.
However, some people with hypersomnia will not have an underlying medical condition and there will be no obvious explanation for it – they have it throughout the day, despite sleeping for a very long time at night. This is known as “idiopathic” or primary hypersomnia.
The rest of this page focuses on idiopathic hypersomnia.
Signs and symptoms
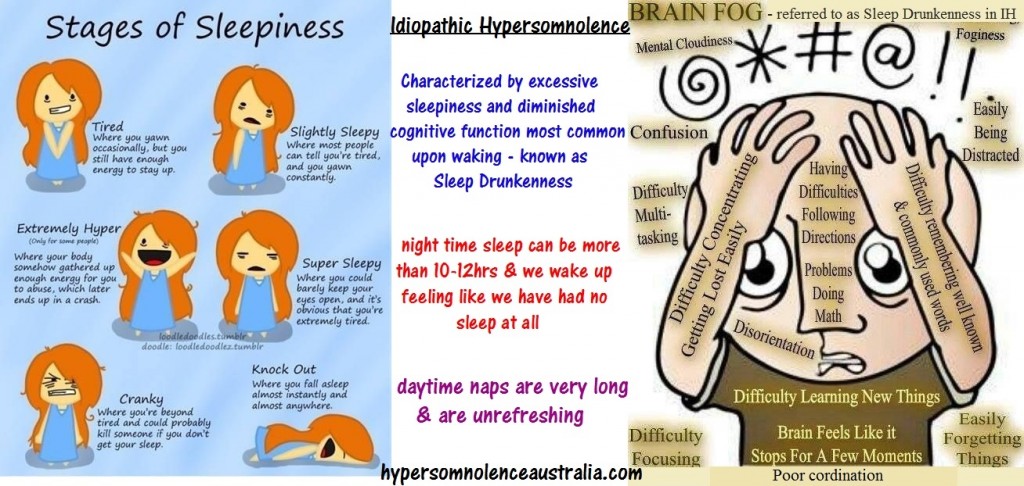
People with idiopathic hypersomnia struggle to stay awake during the day and are usually compelled to take frequent long naps. These may be prolonged or at inappropriate times – such as during a conversation or meal, or even while driving – and generally don’t provide any relief from the sleepiness.
Most people with idiopathic hypersomnia also sleep for more than 10 hours a night and struggle to wake in the morning, because they feel very drowsy and confused upon waking (“sleep drunkenness”), although some people sleep for a regular amount of time (about eight hours) and are able to wake relatively normally.
The excessive sleepiness may have a negative impact on the person’s work, relationships and social life, and they may also:
have mental health problems, such as anxiety or depression
have low energy
be restless or agitated
think or speak slowly
have trouble remembering things or maintaining concentration
perform behaviours around the house as if on “autopilot”
These symptoms often develop during adolescence or in a person’s early twenties, although they can occur earlier or later in life.
What to do
See your GP if you’re constantly drowsy during the day and it’s affecting your everyday life. They’ll want to know about your sleeping habits, how much sleep you get at night, if you wake during the night, and whether you fall asleep during the day.
They will also want to know if you have any emotional problems, such as depression, or if you’re taking any medication that could explain your hypersomnia.
Your GP may also suggest keeping a diary of your sleeping patterns and sleepiness levels for a few weeks, or filling in a questionnaire called the Epworth sleepiness scale to assess whether you’re excessively sleepy during the day.
If necessary, your GP can refer you to a doctor specialising in sleep disorders for tests to help diagnose the cause of your symptoms.
Seeing a sleep specialist
A number of tests can be carried out to assess your sleep and help identify any underlying cause. These are usually carried out at a specialist sleep centre.
Two of the main tests used are:
Polysomnography (a night time sleep test), which will help rule out sleep disorders such as narcolepsy or sleep apnoea. You stay in a special bedroom and are observed from another room through the night. Electrodes are attached to your face, head and body to record brainwaves, muscle activity, eye movement, breathing and snoring.
Multiple sleep latency test – this test usually follows the next day. You’ll be asked to take several naps throughout the day, so doctors can see how long it takes you to fall asleep when instructed (this shouldn’t take longer than eight minutes for someone with hypersomnia).
Doctors may diagnose idiopathic hypersomnia if you have excessive daytime sleepiness and need regular daytime naps, but no other cause is found.
Managing idiopathic hypersomnia
Idiopathic hypersomnia doesn’t usually get better by itself. Many people find that the symptoms improve with treatment.
Medication
There are no medicines specifically designed to treat idiopathic hypersomnia, but medications used for narcolepsy can often help.
The main medications used are stimulants, such as modafinil, dexamphetamine and methylphenidate, which help to keep you awake during the day. See treating narcolepsy for more information on these medicines.
Antidepressants may be prescribed if emotional problems are interfering with your sleep.
A medicine called flumazenil has been shown to help some patients with idiopathic hypersomnia, although more research is needed to be sure of its effectiveness.
Lifestyle changes
It may also help to adopt good sleeping habits, such as avoiding alcohol, caffeine and medications that make the condition worse, sticking to a bedtime routine, and avoiding working at night or engaging in social activities that delay bedtime.