“Everyone has a doctor within them.” Those words — from ancient Greek physician Hippocrates — are proving increasingly true as physicians learn more about using a patient’s own cells effectively to treat peripheral joint pain and disorders that disable millions of Americans, says interventional spine and pain management specialist Jason Arora, DO.
New, promising treatment approaches include injecting a patient’s own blood plasma or stem cells directly into a diseased peripheral joint, explains Dr. Arora, a physician and member of the team at Atlantic Spine Center, with offices in New Jersey and New York.
Peripheral joints refer to shoulders, hands, wrists, hips, knees, ankles and the body’s several hundred other joints not spine-related.
“Blood plasma is rich in antibodies, enzymes and proteins – growth factors — that accelerate healing,” Dr. Arora says. “Adult stem cells, on the other hand, can be harvested from a patient’s bone marrow or adipose – fat – tissue and are regenerative; they stimulate restoration and regrowth of collagen within a diseased or damaged joint.”
In some cases, physicians employ a combination of stem cells and platelet-rich plasma (PRP) to treat peripheral joint problems because they believe the plasma helps maximize the effects of the stem cells, Dr. Arora says.
Ongoing development of these minimally-invasive, biologic therapies has both scientists and physicians — like Dr. Arora — particularly hopeful about the possibility of bringing future relief to almost any patient who suffers from the swelling and pain of common joint conditions like osteoarthritis, rheumatoid arthritis, fibromyalgia and bursitis.
Between 2013 and 2015, more than 54 million adults in the United States were diagnosed annually with some form of joint arthritis – a number expected to rise to 78 million by 2040 as the population ages, according to the Centers for Disease Control and Prevention. Even more troubling, arthritis and other peripheral joint disorders are:
A leading cause of work disability.
Result in severe pain in a large percentage of patients.
Limit the activities of nearly 24 million Americans aged 18 and older.
Cost the economy more than $300 billion each year in medical expenses and lost wages.
Not every expert, however, is excited about PRP and stem-cell therapies. Critics point to several clinical studies that indicate PRP injections may have no greater effect than a placebo. In other research, PRP and stem cells proved beneficial to some patients but not everyone.
Authors of a study in a 2017 issue of Current Sports Medicine Reports emphasize caution in use of cell-based therapies to treat joint injuries in children or adolescent athletes until more is known about the long-term safety and effectiveness of these approaches. They also call for “more regulatory oversight” of biologic therapies and establishment of a patient registry system to catalog treatment and outcomes data.
Dr. Arora concurs that more research is needed but says a growing body of evidence supports the potential benefits of biologic approaches to treating joint problems.
Scientists theorize that, in cases of joint osteoarthritis, which is caused by advancing age, injury or genetic predisposition, stem cells may work by developing themselves into needed cartilage cells or by releasing proteins that slow the degeneration of joint cartilage.
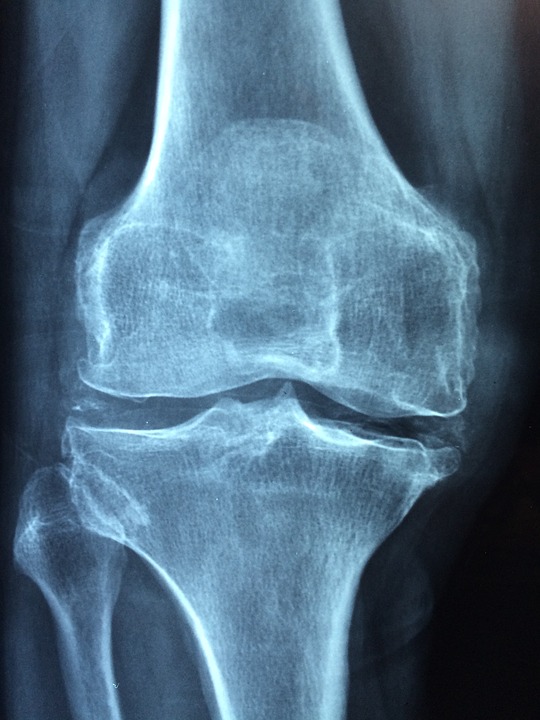
Cartilage acts as a shock-absorber and lubricant for joints, Dr. Arora says. As osteoarthritis erodes cartilage, bones begin rubbing on bones, causing swelling and inflammation in the joint.
“Even after a diseased or injured joint is repaired, prior damage to the cartilage may continue an ongoing cascade of cellular degeneration in the joint,” Dr. Arora states. “That’s why continued study of molecular and biologic treatments, including the potential ability of primitive stem cells to change into cartilage cells, is so important.”
Of course, developing painful osteoarthritis and other disorders of the peripheral joints does not have to be an inevitable result of growing older. Dr. Arora offers these tips to help preserve joint viability:
- Lose weight. Every pound shed removes four pounds pressure from the knees.
- Don’t just sit there. Move. Change positions frequently. Stay active.
- Protect joints during sports activities. Wear elbow and knee pads or knee braces, for example, depending on the sport.
- Reduce risk of falls and other joint injury by strengthening back and abdominal muscles.
- Participate in low-impact activities like swimming or walking.
- Practice good nutrition. Eat foods that promote healthy bones.
- Stop smoking and limit alcohol consumption.
Atlantic Spine Center is a nationally recognized leader for endoscopic spine surgery with several locations in NJ and NYC. http://www.atlanticspinecenter.com, http://www.atlanticspinecenter.nyc