Planning for end-of-life care is an essential part of managing senior health. Creating advanced directives, commonly known as living wills or advance decisions, ahead of time makes it easier for seniors to appropriately budget for palliative treatments or hospice services, reducing the burden on family and caregivers. Take advantage of how seniors are staying active longer, and use the time to take charge of your end-of-life care for greater independence and to ensure your wishes are respected when advanced directives are required.
Staying Active Longer
Seniors are more active than ever, and staying active longer enables those aged 65+ to take a bigger role in managing their end-of-life plans. This gives seniors the opportunity to seek out trusted advice on managed healthcare (debunking myths that can prevent informed decisions) and get realistic quotes to set expectations for expenses.
Technological advances in care for the elderly can keep seniors involved and able to enjoy active lifestyles. According to the University of Illinois at Chicago, internet usage is on the rise among seniors. Elderly patients can take advantage of online health monitoring tools, participate in social communities with others who share similar interests or health conditions and even get real-time wellness feedback using wearable devices. All of these advances make it easier to more accurately determine end-of-life needs.
Establishing an Advanced Directive
Advanced directives explain your wishes for care when you are unable to communicate them due to illness or injury. These directives are not always focused on life support, but can also include key decisions such as the types of treatments provided (surgical, nonsurgical, experimental, holistic) and set durations for treatment. Advanced directives can also establish proxies, transferring power of attorney over medical decisions to trusted family members or friends.
Doctors do not turn to advanced directives for momentary lapses or temporary conditions. Many states require terminal illness or permanent unconsciousness before physicians may allow advanced directives to trump standard practices. This ensures that patients are given every chance at recovery before doctors enact these planned decisions. State laws vary on the witness requirements for certifying advanced directives, but none require a lawyer or any additional fees for filing.
Preparing for Hospice
Hospice caregivers help assist those suffering from terminal illnesses with no known cure. Since heart disease, cancer and diabetes are such common causes of death, hospice services are typically available for sufferers who have a diagnosis that puts the end of life within six months. The major difference in this type of healthcare versus normal treatment is that pain management and ensuring quality of life takes precedent over recovery. Regular monitoring and attention to progression are hallmarks of such care. These services regularly include end-of-life counseling and advice for estate planning and are regularly extended to family members.
According to the University of Southern California, hospice services often offer respite care for family involved in caregiving. Respite plans include regular checkups by health professionals at home or in a managed-care environment and a specific amount of time spent taking the load off of those who normally attend to elderly or ill family members. This pre-arranged service helps relieve some of the stress and strain associated with ongoing caregiving.
Agreeing on When to Act
The best time to create advanced directives and decide on end-of-life care is as soon as possible. Illness and injury can strike at any time, and seniors are likely to face additional challenges over time. Falls pose a serious risk for elderly patients, leading to severe injury or even death, making it more important than ever to have such directives in place.
Caregivers should remain alert for the signs that a senior needs help and never shy away from important end-of-life discussions. Elderly patients may wish to avoid being seen as dependent on others, making it important for caring loved ones to reach out and assist as they can with getting advanced directives established. Agreeing on what signs should result in actively seeking end-of-life care from established providers and when to seek to enforce living wills can reduce stress when the unforeseen arises.
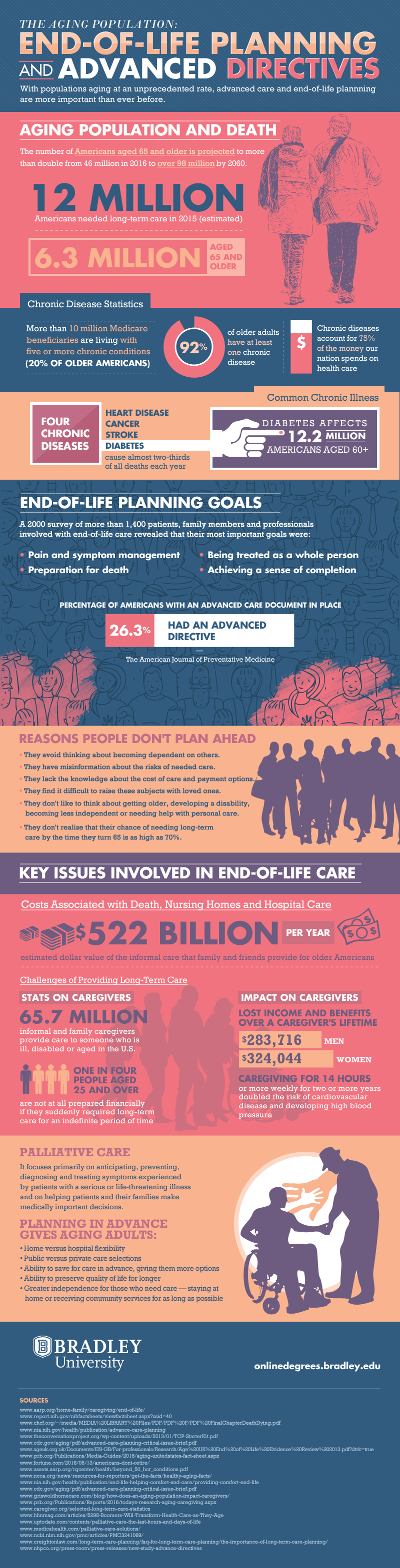
For more information, check out Bradley University’s Online Nurse Practitioner programs “The Aging Population: End-of-Life Planning and Advanced Directives” graphic.