1. Shingles
Shingles is one of the most painful medical conditions you can be unlucky enough to experience. Caused by the varicella-zoster virus, which also causes chickenpox, it’s characterised by a rash or crop of blisters on one side of your body, often around the waistline.
The pain of shingles tends to be burning or tingling and often affects only one side of your body. It can be so bad that you experience an excruciating stab of pain when someone simply brushes lightly against the affected skin or a breeze wafts over it.
Some people who have had shingles can develop a persistent pain called postherpetic neuralgia.
Read more about shingles and the shingles vaccine.
2. Cluster headaches
Imagine giving birth without painkillers once or twice a day for up to 10 weeks at a time and you have some idea of the sheer misery of cluster headaches.
Cluster headaches are also called ‘suicide headaches’ because they’re so excruciatingly painful they’ve been known to drive people to take their own lives. They tend to come on very suddenly without warning causing a sharp, stabbing pain around one eye. Attacks can be as short as 15 minutes or last three hours or more.
They’re acknowledged to be the most painful type of headache, worse even than severe migraines. In fact, experts have suggested that cluster headache may be the most painful condition known to medical science.
Read more about cluster headaches.
Find your local headache clinic.
3. Frozen shoulder
This condition isn’t just extremely painful, it can also last for several years unless it’s properly treated.
In frozen shoulder, the joint becomes so tight and stiff that it’s virtually impossible to carry out simple movements such as raising your arm. Daily activities like taking off a T-shirt, lifting a kettle, putting on a coat, even combing your hair, become an ordeal.
It’s not clear what causes frozen shoulder, but it can happen after a shoulder or arm injury and is more common in people with diabetes.
Either shoulder can be affected but it’s usually the non-dominant one – that’s your left shoulder if you’re right handed or your right shoulder if you’re left handed.
Pharmacy or prescription painkillers usually help, along with shoulder exercises.
Read more about frozen shoulder.
4. Broken bones
A broken or cracked bone is known as a fracture. Common examples are broken ankle, broken hip, broken arm and broken nose.
If the break is small, it’s possible not to feel any pain at all, but generally it really hurts to break a bone, especially when you try to move it. The pain is often described as feeling like a deep ache.
Broken bones can heal by themselves, but they may need to be lined up and fixed in position so they set properly. As a general rule, the older you are and the bigger the bone that’s broken, the longer it will take to heal.
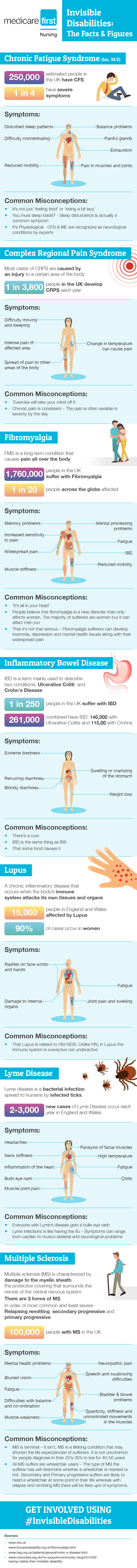
5. Complex Regional Pain Syndrome (CRPS)
With Complex Regional Pain Syndrome (CRPS), a severe pain follows an injury to bone and soft tissue. It can happen to anyone at any age, but is most common in women in their 40s and 50s.
The burning pain of CRPS is continuous and intense, often out of all proportion to the severity of the original injury. It usually affects one of the arms, legs, hands or feet.
Often the pain spreads to the entire arm or leg, even though the initial injury might have been only to a finger or toe. Sometimes, the pain even travels to the opposite extremity.
The pain of CRPS can go on for years, and there’s currently no cure as such. Treatments, such as physical therapy, talking therapy and medications, aim to help those with CRPS get on with their lives.
Read more about CRPS.
6. Heart attack
If you have a heart attack, you usually get a pain in the centre of your chest – often described as a sensation of heaviness, tightness or squeezing that can be so bad it causes you to collapse.
The pain can feel like really bad indigestion and sometimes spreads to your jaw, neck, back, arms or stomach.
If you suspect you or someone else is having a heart attack, call for emergency help straight away.
Read more about heart attack.
Read 64-year-old Derek’s real-life description of what it feels like to have a heart attack.
7. Slipped disc
Back pain affects eight out of 10 people at some point in their lives and one of the most common causes of back pain is a slipped disc, often the result of a twisting or lifting injury. What happens in this medical condition is that one of the discs in the spine ruptures and the gel inside leaks out.
Most people with a slipped disc experience sudden and severe lower back pain, which is usually eased by lying down and is often made worse if you move your back, cough or sneeze. A slipped disc can often cause leg pain as well as, or instead of, back pain.
In most cases of slipped disc, the pain eases gradually over several weeks. Painkillers can help.
Read more about slipped disc.
8. Cancer
Most people with advanced cancer experience pain, either from the tumours themselves or as a side effect of cancer treatment such as chemotherapy or radiation.
Although the pain can be very severe, it doesn’t always mean the cancer is growing. A very small tumour that is pressing on a nerve can be agonising, while a large tumour somewhere else may cause little or no pain.
Cancer pain can vary in sensation, duration and intensity depending on the type of cancer you have and the stage that it’s reached, but it’s almost always possible to get cancer pain under control with prescribed painkillers.
Read more about cancer.
Find your local cancer support services.
9. Arthritis
People with arthritis endure constant and often agonising joint pain, usually in the hips, knees, wrists or fingers.
The pain can come on suddenly or over time and is often linked with muscle aches and stiffness in the joints.
Various different types of arthritis can cause joint damage, including rheumatoid arthritis, osteoarthritis and lupus.
According to Arthritis Care, whatever type of arthritis you have, exercise is one of the best ways to keep pain at bay. Your doctor or a physiotherapist can help you pick an exercise programme that will suit you.
Read more about arthritis.
Find your local arthritis support services.
10. Migraine
A migraine headache is much more painful than a conventional headache and tends to last for longer, with the worst ones persisting for up to three days or more.
Because migraines can cause vomiting and extreme sensitivity to light and sound as well as intense throbbing pain, all that many with migraine can do is find a dark, quiet place to lie down until their headache is over.
Medications can help reduce the frequency and severity of migraines. If treatment hasn’t worked for you in the past, talk to your doctor about trying a different migraine headache medication.
Find out more about migraine and read a true-life account of what it’s like to have migraine.
Find your local migraine clinic.
11. Sciatica
Sciatica is the name given to an aching pain running down the leg. It’s caused when the sciatic nerve – the longest nerve in the body, which stretches from your back to your feet – has been pinched or irritated by damage to the back. It’s often caused by a slipped disc.
Sciatica is different to general back pain – the pain of sciatica hardly affects your back at all but instead radiates out from your lower back, down the buttocks and into one or both of the legs, right down to the calf.
Most people find their sciatica goes away by itself within a few days or weeks. A combination of self-help measures such as over-the-counter painkillers, exercise and hot or cold packs can usually relieve the pain in the meantime.
Read more about sciatica.
Watch this video of one man’s experience of the pain of sciatica.
12. Kidney stones
Passing a kidney stone produces a sudden, incredibly sharp, cramping pain in your lower back or the side of your abdomen, or occasionally in your groin, which may last for minutes or hours, with pain-free intervals in between.
The pain often begins in the middle of the night and can be so vicious that those who experience it may feel the need to go to A&E.
In fact, most kidney stones will be small enough to be passed out in your urine at home – and thankfully the pain disappears once the stone has been passed.
Read more about kidney stones.
13. Appendicitis
Appendicitis is a painful swelling of the appendix, a finger-like pouch attached to the gut wall. It’s most common in children, who typically complain of pain in the middle of their tummy that comes and goes. The pain then shifts to the lower right side of the tummy and gets a lot worse.
Appendicitis is a medical emergency that usually needs an urgent operation to remove the appendix before it bursts.
Most children recover from having their appendix removed within a few days and experience no ill-effects from the operation.
Read more about appendicitis.
Watch this animation to learn about the causes and treatment of appendicitis.
14. Trigeminal neuralgia
The pain of trigeminal neuralgia is often described as feeling like an electric shock shooting through the face. Others have described intense sensations of burning or stabbing. They often describe a trigger area on their face that’s so sensitive that touching or even air currents can trigger an episode.
Trigeminal neuralgia, also known as Fothergill’s disease, is characterised by bouts of extremely severe one-sided facial pain that comes and goes unpredictably in sudden attacks.
Usual painkillers have no effect, but prescribed anticonvulsant drugs (used for epilepsy) can dampen the pain.
Read more about trigeminal neuralgia.
15. Pancreatitis
Pancreatitis is inflammation of the pancreas, a banana-sized organ that’s part of the digestive system, and its most common symptom is awful abdominal pain.
It can happen as a one-off event (acute) or the pancreatitis can keep coming back (chronic). Acute pancreatitis, though, is more painful and is often a medical emergency needing hospital treatment, including to control the pain.
The pain of acute pancreatitis is similar, and easy at first to confuse with, that of another painful and serious condition called cholecystitis, where the gallbladder becomes inflamed, usually because of gallstones.
Read more about pancreatitis.
16. Gout
Gout is one of the most painful forms of arthritis where swelling and severe pain develops in a joint, often the base of the big toe, to the point where even touching or moving the toe can be agony.
Many people associate gout with Henry VIII and good living, but it’s a myth that gout is caused by binge drinking and gorging on rich food. Although it’s more likely in people who eat a lot of red meat and drink beer, anyone can get gout, even teetotal vegetarians!
According to Arthritis Care, in an attack of gout the joint starts to ache then swells up and becomes red, hot and extremely painful. The joint may look as if it has a boil on it, or the skin can become shiny and peeling.
An attack can last between one and 10 days. There can be permanent damage to the joint if you get recurrent attacks, so it’s wise to consider medication to stave off further bouts.
Read more about gout.
17. Endometriosis
One in 10 women in the UK experiences the painful gynaecological condition endometriosis, where cells like the ones in the lining of the womb are found elsewhere in the body.
While some women with endometriosis have no symptoms at all, others have lots of pain – pelvic pain, period pain and pain during and after sex.
Although there’s no cure for endometriosis, there are treatments that can relieve the pain and shrink or slow endometriosis growth.
Here, Michelle, a mum of two, describes life with endometriosis.
Read more about endometriosis.
18. Stomach ulcer
An ulcer is a sore or hole that forms in the lining of the stomach. For the one in 10 of us that will have a stomach ulcer at some point, it causes a gnawing or burning pain in the abdomen, often between meals and in the early hours of the morning.
Ulcer pain is usually relieved by eating or taking a type of medicine called antacids.
It’s important to take your medication because an untreated ulcer can become perforated, which is an excruciatingly painful medical condition where the ulcer burns through the stomach wall letting digestive juices and food leak into the abdominal cavity. A perforated ulcer is a medical emergency and usually needs to be operated on immediately.
Read more about stomach ulcer.
19. Fibromyalgia
The exact cause of fibromyalgia isn’t known but it can cause widespread aches and pains all over the body, usually as lots of tender areas on the back of the neck, shoulders, lower back, hips, shins, elbows and knees. People with fibromyalgia often say they ache all over.
Quite often the pain and stiffness is worse in the morning and you may have more pain in muscle groups that you use repetitively.
While fibromyalgia is a lifelong condition, treatment including painkillers and exercise, can ease discomfort.
Read more about fibromyalgia.
20. Pain after an operation
It’s common to have some pain after surgery, though the intensity of the pain will vary according to the type of operation.
But too much pain after surgery is not a good thing and you should never feel you have to ‘tough it out’.
There are lots of effective painkillers on offer to keep your pain after surgery under control, and, in addition to making you more comfortable, experts say that well-controlled pain will help you get better faster and prevent long-term problems.
Read more about what happens after having an operation.