Brain fog
As regular readers of this blog know for many years I worked in the area of healthcare and medical market research. For many conditions such as Multiple Sclerosis, Rheumatoid Arthritis and Fibromyalgia patients often reported what may refer to as “brain fog”.
However this symptom, according to my research participants, was ignored or unmentioned by the medical profession. The purpose of this discussion blog is to allow our readers to share in more detail their experiences of brain fog and its impact on their lives and their loved ones.
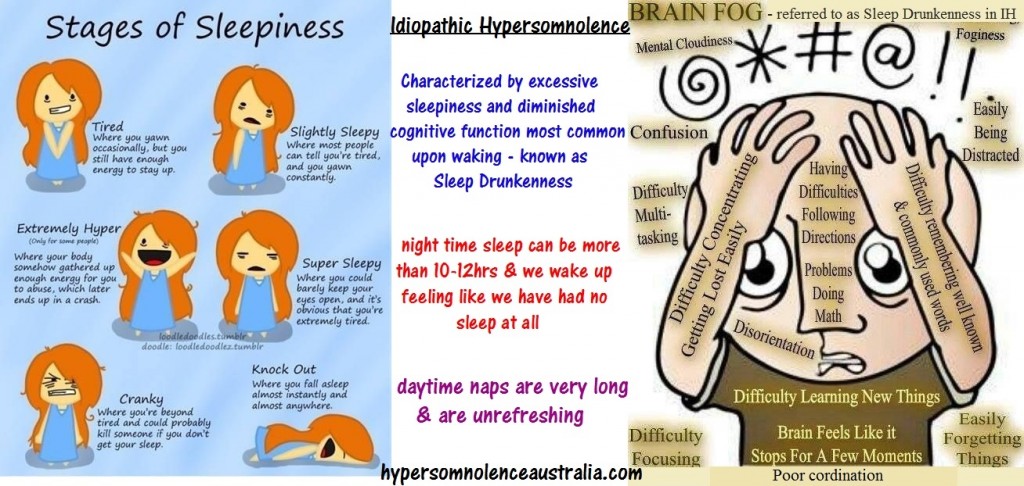
So what actually is brain fog?
There seems to be no clear clinical definition but a good description might be clouding of consciousness. A term which was originated in the nineteenth century to describe low level cognitive impairment in different kinds of patients.
Typical symptoms of brain fog include:-
a) Poor memory function.
b) Difficulty in concentrating.
c) Problems with learning new things.
d) Inability to find/remember the word you are “looking for”.
You may wish to consider answering the following questions?
1) What are the main symptoms of your brain fog?
2) What do you think is the underlying cause of your brain fog?
3) Please can you describe the impact of brain fog upon your lifestyle?
4) How do you deal with brain fog? What if any treatments do you use? Have they had any success?
5) Can you suggest any useful online resources for people with brain fog?
6) Why do you think little attention is paid to brain fog by healthcare professionals? If, on the other hand you feel that it is well covered by your medical support please tell us a bit more.
Thanks very much in advance for all your help with this discussion blog.
Here are just a few of the responses!
“1) What are the main symptoms of your brain fog? I can be in the middle of speaking and stop mid sentence and forget what I am talking about. Often. I have problems word finding. I cant remember simple things. I cant remember any names whatsoever. even if i have known someone for 20 years. I cant problem solve as well as I used too. I have a bit of delay when people say things to me often. Sometimes I remember a random childhood event out of nowhere. I try to write it down because im so afraid i wont think of it again and that i will loose memory. I can not recall things. That is one of the hardest things for me to do is recall things. Whether it be a date, number, person, event. Anything. It is awful. I hate it.
2) What do you think is the underlying cause of your brain fog? Fibromyalgia. and ptsd
3) Please can you describe the impact of brain fog upon your lifestyle? It is horrible. It has gotten worse this past year and truly affects me daily. I struggle to do things at work that I used to do with ease. I feel way to young to have these issues.
4) How do you deal with brain fog? What if any treatments do you use? Have they had any success? I write EVERYTHING. I write every single thing i can down. i have so many notebooks. I do not have any other treatments really other then trying to reduce stress which is an ongoing task.
5) Can you suggest any useful online resources for people with brain fog? no but it would be nice to find something.
6) Why do you think little attention is paid to brain fog by healthcare professionals? If, on the other hand you feel that it is well covered by your medical support please tell us a bit more.
I feel that brain fog is often ignored by health care professionals for a few reasons. Personally, I feel that they just dont believe me. I am only 24 and try to tell them how bad it is. I feel like it hasnt been taken seriously for a long time. Many misdiagnose it seems. Yes Depression is a nasty thing and causes similar symptoms, but this is different.”
“As the mother of a formerly bulimic daughter (7th-10th grade, now a mom herself). I can assure you that if you also tell your parents everything they will take you seriously. My daughter was taking diet supplements and I know that she was purging but for the life of me could not get her to stop. She denied it and denied it until she began having health problems. She has a twin sister and I do not know if I would have ever learned about this had her twin sister not told me. The advice the other lady gave you is only partially correct. If you are doing something to harm your self the doctor is obligated to discuss this with your parents. Would you not rather this information come from yourself? And this is only true if you are below the age of 17 and from what I understand you should be. Your parents are not listening to you because all they are seeing is that your your grades have dropped and the fact that you were previously a straight a student SHOULD tell them something is wrong. However parents are not perfect and sometimes they get wrapped up in their own lives and preferred to push an issue under the rod until it is staring them right in the face.
Trust your parents sweetheart. They love you and only want what’s best for you even if they have been blind to the situation. I fully believe that if you are completely honest about EVERYTHING; with your parents doctor or whomever you choose to tell, that no one is going to tell you that it is just in your head.
If you need help speaking to your parents prior going to see a doctor I suggest going to your assigned school counselor and speaking to them first. Ask him or her to sit in on a conference with your parents. This will also show the parents that you feel like you have not been heard. Because you went to the counselor first they will also understand the gravity of the situation and take you very seriously. I’m sure they want to get you the help you need but they do not have knowledge of just how serious the issue is because you are only telling them about the symptoms but not what is causing those symptoms. Because of the way who told your story I believe you know deep down why you are experiencing Brain Fog. Zoning out and not being able to remember where you are or what you’re doing is a black out and if you are driving during this time, you could not only take your own life but someone else’s as well and I know you don’t want to hurt anyone.
If I remember reading correctly, I believe you said your aunt gave you food. Maybe you can have your aunt sit down with you and your parents while you tell them about your dieting; if you do not feel comfortable with the school counselor. However, as a parent I just feel like it would show a little more gravity to the situation if it were to involve the school counselor. It was a call from a school counselor telling me they noticed differences in my daughters behavior and what they suspected which first brought my attention to it, then her sister confirmed what she knew when I asked her if she had noticed. I knew both of them had been losing weight. But they had joined the swim team and I just assumed it was because of that.
Understand there is only a certain amount of information that any doctor can share with a parent; a medical doctor that is. If you were to go to counseling after all tests have been ran and ruled out any other medical problem with your brain …don’t be afraid that those sessions would be discussed with your parents. I never learned anything that was discussed in my daughters counseling sessions; but she did get better. I will be praying for you and for God to lead you and guide you to get the help you need. You are to young and to smart to be going through this. I’m proud of you for reaching out on this blog now the rest is up to you.
God be with You!”
“In addition to my post below, here is my response
1) What are the main symptoms of your brain fog?
i used to feel very cloudy and almost like a headache. my brain just felt fragmented like the computer definition. It felft like a struggle to apply myself cognitively
2) What do you think is the underlying cause of your brain fog?
a variety of factors, including poor digestion, definitely poor sleep but my current hypothesis is that I didnt have the right ‘brain stimulation’ ie my brain was very ‘unfit’
3) Please can you describe the impact of brain fog upon your lifestyle?
It stopped me progressing at work. I stuggled to apply myself in challenging tasks. I was also quite miserable.
4) How do you deal with brain fog? What if any treatments do you use? Have they had any success?
Two things had major success for me. 1. Properly engineered brainwave entrainment – particularly the key track off WorkSharp from ActiveMindsGlobal.com; and 2. the right nutrients, specifically a bio-active b vitamin complex, omega 3 fish oil and magnesium.
5) Can you suggest any useful online resources for people with brain fog?
Two key resources:
http://www.activemindsglobal.com/
http://www.drmyhill.co.uk/wiki/Brain_fog_-_poor_memory,_difficulty_thinking_clearly_etc
6) Why do you think little attention is paid to brain fog by healthcare professionals?
Because it’s very hard to quantify or qualify the symptoms. Even a slight change in your energy output through diet, stress, lifestyle factors, poor sleep etc can substantially affect cognitive function. Also Neurologists would be the only doctors that come close but they don’t seem to focus on subjective symptoms such as clarity of thought, memory recall, cognitive processing speed etc.”
“1. Can’t read a book, can’t recall what’s happened in a tv series/soap, feel slightly detached from reality… a bit ‘cotton woolly’….
2. Stress, depression, menopause, hereditary.
3. Loss of feelings, don’t enjoy anything anymore, worry unnecessarily about things, tearful and anxious, feel vulnerable, upset at forgetting things.
4. Just try to work through it, try different diets, avoid situations where I feel vulnerable/stressed.
5. I write down important things
6. I have never been to Drs about it as I don’t think they would take it seriously!”
“1. Flustered, irritable, impatient with self for not remembering
2. Fatigue, Heat, Medication, Sensory Overload
3. Conflict, Lowers Self Worth, Second-guess oneself, automatically believe YOU must be at fault
4. REST and maintain an ambient temperature
5. No, I have ONE place where I write my “reminders” – I have RRMS for 14 years
6. The embarrassment of admitting you have brain fog and not wanting to know about it”
“There are many reasons for brain fog and age is certainly not one of them! I’ve known people and have relatives that are well into their 80’s and even 90’s who are sharp as a tack. What we eat (nutrition) has a lot to do with brain function. Being overweight as so many are doesn’t help. There are studies and research being conducted that suggest that toxins being released through our intestinal wall enters our blood stream and can damage not only our body but our brain. Exercise and diet have a lot to do with being healthy in body and mind. Avoiding all the GMO and contaminants certainly can’t hurt. I have Celiac Disease, Chronic Fatigue and Fibromyalgia along with brain fog. I’ve discovered changing my diet, becoming way more health conscience regarding exercise and diet and shedding a few pounds has made a huge difference for me. At 55 I’m not ready to concede. Age is only a number! Dementia and MS took it’s toll on my mother in her latter years, I don’t want to burden my children with what we had to go through with my mom. Eat right and exercise!”
“I too am like this all of the time. I am 65 so that is to be expected I suppose. The problem is that I have been that way since I was in my thirty’s….I even went to a physiatrist about it. She suggested keeping a notebook with me all of the time. Writing down where I parked , what I came to the store for,etc. That along with having a GPS has saved my life. I have to wonder if we try to overload our brains to the point nothing sticks there permanently . I know when people are talking to me I am thinking of other things at the same time and do not hear all they are saying. I have found by writing down a lot of the things I need to remember that I am no longer thinking of them subconsciously and am able to focus better …It is worth a try ! It makes me so much less stressed.”
“Brain fog – Good word and nice to know that I am not the only one who suffers from this. To sum it up for me: embarrassing; humilitating; frustrating; depressing and most of all so damn scary! It has got to the point where I make excuses not to drive because I fear losing my boundaries begind the wheel. Typing – forget it – so many errors. Fingers just do not want to go where they are suppose to. The more I try to concentrate, the worse it gets. I also get told that I am very hot-headed. Well for those of us who suffer from any symptom of MS we know that pain is a daily thing we face and generally we have to face it alone . We do not have”tempers” we just have a difficult time trying to convey our messages.”
“Main issues:
I cannot keep track of anything that has to do with numbers ei. dates, times, simple math, addresses, and phone numbers. My children find themselves frustrated at me because they have to repeat most of what they say to me at least twice. Depression. Can’t get a job with benefits due to pre-existing condition.
Underlying cause:
Very poor nutritional values.
Impact on lifestyle:
Unable to obtain a job.
Very low self esteem due to depression.
How do I deal:
The Wahls Protocol by Dr. Terry Wahls
I try to improve my lifestyle.”
“First, don’t panic! I hardly think this is an early sign of dementia! MS lesions can affect the brain and cause cognitive issues, but it sounds like you have lesions like I do, on the spine. In all the research I’ve done, it’s quite common for anyone with an auto-immune disorder to have the fatigue and brain-fog. Personally I think it’s because our bodies have to work so much harder to keep us going through normal life! It’s maintaining us while also coping with a disease. So, number one on my list is to get enough rest. Eat a healthy diet. Get enough moderate — not intense — exercise — and make lots of lists so I don’t forget important stuff. I laughed when I saw your note about leaving car doors open. I did that just recently. This is pretty minor — and it isn’t just those of us with chronic illness that do that — anyone over 50 will tell you they do this, too. Forgetfulness is a fact of aging as well. I am 54. A lot of my friends laugh when I tell them what I do and they say, yeah, I do that and I do not have MS. So they are helpful to me in giving me some perspective. Be kind to yourself. We have more to cope with than most people. If you can cut back on what you have to do on a daily basis, I find that limiting the number of things I have to do each day helps me not be so forgetful. Write stuff down. Take naps. Do one activity before starting another. Try not to be put in situations where you are multi-tasking. I get some helpful supplements from my naturopath that support me energetically. That might be worth a try for you, too. Avoid alchohol — drink sparingly because it will tire you. I limit caffeine, too, because of the post-caffeine let-down. But I use it in the morning. Hope that helps.”
“My husband age 63 (now ). In 2007 he started having periods of forgetfulness, extremely poor memory, hand tremors (slight), falling, bumping into things short term memory loss, slurred speech! In 1999 he stated chemo. For Non- Hodgkin’s lymphoma. He tolerated it pretty well and even worked a little. 2007 he got mono after the flu. He was in bed, ate & bed. He was diagnosed with chronic fatigue,2009 chemo. For B cell non- Hodgkin’s . It took care of the CA. But he has not be well since! We started going to all types so specialists. He has had brain fog since 2007 but it has progressed! He doesn’t ‘t do anything. He won’t shower! He eats sleeps, watches T.V. Then the cycle starts over again! The neurologist ruled out Parkinson’s .he has sleep apnea, uses a C Pap with oxygen but has interrupted sleep. The Geriatric psychiatrist had him straighted out for awhile. He changed his depression meds. Around and he started doing better. Now, after several surgeries (general anesthetic and three procedures for nerve impingements () and some dental work () he started going through brain fog, tripping and everything is a mess again! Any Comments…..I am tired! I want to help him! My daughter came up with Caine allergy! We have yet to speak to the Dr. He has upcoming appointments. GB!
“I get lost in the middle of conversations because my mind seems to literally go blank. I can’t remember what I was saying, and I can’t remember what we were even talking about. Sometimes I realize in the middle of someone talking to me that I lost track of the conversation and I have no idea what they are saying to me. I have a very hard time pulling out names, even of my own children. Often times I will rotate through four or five names before I get the right one, and thats if I get the right one; sometimes I just give up. I have a hard time focusing on what I am doing, but again, this is particularly bad with conversations. At work, I have a hard time completing tasks if people interrupt me in the middle of what I am doing because I get side tracked. Just the other day I had a particularly emotional(angry) outburst at a coworker because she kept interrupting me and repeating herself so I snapped and just said forget it, that isn’t what Im saying and Im done trying to rephrase it. It’s very frustrating and it affects my daily life. I am constantly struggling for words, struggling for names, and struggling to recollect memories from my short term memory.”
‘Brain Fog’…more like Brain Blizzard
1) What are the main symptoms of your brain fog?
A) Memory retention and concentration/focus problems.
2) What do you think is the underlying cause of your brain fog?
A) Secondary Progressive Multiple Sclerosis
3) Please can you describe the impact of brain fog upon your lifestyle?
A) I tend to stay home most days; when there’s a job interview, I usually panic and either go or ditch the entire uncomfortable experience.
4) How do you deal with brain fog? What if any treatments do you use? Have they had any success?
A) How does anyone ‘deal’ with this? There are currently no treatments for this ‘brain fog’.
5) Can you suggest any useful online resources for people with brain fog?
A) No.
6) Why do you think little attention is paid to brain fog by healthcare professionals? If, on the other hand you feel that it is well covered by your medical support please tell us a bit more.
A) I often wonder this same thing…if there’s a secret among the medical team, I’m feeling mighty ripped off at this point :/
“I have Fibro, Chronic Fatigue, Myofascial Pain Syndroms, and several autoimmune issues, among other annoying (and boring) deseases. Brain fog has been a major contributing factor to my inability to function and live as independently as I did when I was less ill.
I used to be in software and systems engineering and management, which required a lot of math and statistics, quick strategic thinking and decision making and NO mistakes. I was very successful, very well paid and well respected in my industry. I ended up going from working no less than a 60 hour week to having to go on Disability because I could no longer complete a simple algrorythm, let alone add two numbers. Multitasking was impossible, and I couldn’t stay awake or sit at my desk for more than a 10 minute stretch without having to get up and move.
1. I have all the symptoms listed above. The worst is not being able to recall words or people’s names or the names of things/places. It’s as if there’s a backfire happening in my brain like car, and I just sputter. 2. Lack of REM sleep, too much sugar or other poor dietary choices, increased pain and stress. 3. People often think I have a selective memory, which is maddening. When I find myself lost in places where I know I should know where I am, I can get panicky. Maps don’t make sense to me, and right becomes left, etc. I get angry and frustrated with myself, at times, but mostly I find myself feeling fearful when I cannot remember words or people’s names or I find myself suddenly lost. And forget about learning anything new! I can’t retain anything!Reading books is no longer enjoyable, as a result. 4. and 5. I am not able to provide you with anything that’s useful, I’m sorry to say. 6. Brain fog has never been addressed by any of my specialists in the 20-25 years I have been dealing with it until this padt year when I saw a CNP who specializes in FMS, but it it was an acknowledgement of the issue only.”
“It is horrible, I was a home health nurse, I didRural areas of south dakota. My fog was so bad I would get lost not knowing how I got where I was at or how to get where I was supposed to go. Frightening. I was also having difficulty filling pill boxes, making mistakes and trying to fix them was hard too.I say words I dont mean or cant find the right one to say. I can’t remember diseases and how we treat them or not remembeing little steps in procedures I had done millions of times. I quit the job and let go of my licenceI couldn’t risk hurting someone. With reducing stress it helped alittle I still do things and not remember them. Or words finding the right word to say is really bad and I cant remember names or new people. I think docs dont say anything because they dont know how to treat it. Oh I don’t drive unless someone is with me now which is rare as I dont leave my house much. Life altering.”
“hi I have fibromyalgia tmj cfs ME and degenerative disc disese ibs ius acid reflux & colitis titinitus my specialist has told me that having all these conditions at once has caused a scensory over load to my system giving me brain fog I get blurred vision head aches & then the memory loss forgetting words or what im doin starts I also get confussed & forgetfull & can become disorientated when I get the brain fog I cant stand moise its as tho I have a bubble over my head and every sound is exaggerated 10 times louder this causes a creeping tingling sensation that creeps up the back of my head towards my forehead and gives me a pressure headache that fills like my head wants to explode all I can do when its like this is to lay down in a quiet darkend room when this isn’t possible & you are around people im sure they must all think im very ignorant as I cant seem to focus or follow one conversation at a time I tend to avoid large groups n places that are moisy or if I do go I can only tolerate it for a while & have to leave I no longer can drive due to relapses in my thinking process what if I was to switch of or have a blank moment whilst driving ,,, im hoping once I start getting treatment for some of my conditions & they become managble the brain fog will start to reduce or inhope stop all together my specialist couldn’t give me any indications as to wether or not this will be the case I just have to go through tratments & wait & hope this will get better xxxx”
”
“1) What are the main symptoms of your brain fog?
Short term memory, can’t think forget my words, cannot focus or pay attention for long periods
2) What do you think is the underlying cause of your brain fog?
Chemotherapy and being put to sleep too much due to having several surgeries
3) Please can you describe the impact of brain fog upon your lifestyle?
Caused severe depression and issue with my previous diagnosis of PTSD, Lost my JOB
4) How do you deal with brain fog? What if any treatments do you use? Have they had any success?
Take it day by day and so far nothing has helped
5) Can you suggest any useful online resources for people with brain fog?
Unfortunately not
6) Why do you think little attention is paid to brain fog by healthcare professionals? If, on the other hand you feel that it is well covered by your medical support please tell us a bit more.
I believe most people think it’s an excuse”
“mine started almost 4 years ago. i have cfs and fibromyalgia. but i thought it was alzheimer’s starting at an early age (i’m 53). i gave away my car. i would get lost on streets i grew up driving on. didn’t recognize where i was, and panic and tears would overwhelm me to the point that i thought i was having a heart attack. i started isolating because i was embarrassed that i couldn’t speak a whole sentence without losing my words. i still can’t speak a whole sentence. i get aggravated when i can’t find a word and people get impatient and are no longer interested in what i have to say. i feel unimportant. i want to finish my sentence! my friends have now all fallen away. i can’t cook a dinner without panic. total confusion in the kitchen. when i’m alone, it’s fruit or frozen veggies, mostly. maybe a piece of meat. one thing only, or i lose it. i feel stupid when someone tries to show me new things. it’s like it goes in one ear and out the other. i can’t take ‘focus’ meds, as they make me nervous. i have recurring major depression and anxiety disorder and ‘agoraphobia’…i think that comes from isolating because i don’t want anyone to see what i’ve become. i take the meds and hope for better days. i’m not so sure, though. i just want help. the only person who listens is my shrink, and that’s only because she’s paid to. and even then, i’m not so sure she does. if you only knew how long it took to write this. i need someone to listen and help :'(“