April is Bowel Cancer Awareness Month – Find out the Symptoms of Bowel Cancer here
bowel cancer
Bowel Cancer – signs, symptoms and causes of bowel cancer
Bowel Cancer – signs, symptoms and causes of bowel cancer
Giving a stool sample – a users guide!
Thousands of people every year will be asked by their GP or other healthcare professional to give a stool (poo) sample for testing. A lot of people find the idea of this unpleasant and the pot is small so how do you fill it?
A team in Public Health England’s (PHE) Primary Care Unit in the South West explored some of the barriers to people returning poo samples and have developed a leaflet which will be launched soon to show how it can be done easily and with minimum unpleasantness.
Poo is a very important material for doctors as it can be used to test for a wide range of diseases and conditions. These include salmonella, E.coli, cryptosporidium, campylobacter, and bowel cancer, to name a few.
The team interviewed 26 patients to ask them about their experiences of collecting a poo sample and the responses were analysed by theme.
The main barriers were seen as:
• Embarrassment
• Fear of the results
• Concerns about hygiene and contamination with taking the sample
• Discretion and privacy in the surgery when returning the sample
• Lack of information about how to collect it and most patients emphasised the need for a leaflet
The main reason people would give a sample, despite these barriers, was for personal benefit – they wanted to know the results.
Dr Cliodna McNulty, head of the Primary Care Unit, said: “Although most people think of poo as being disgusting it does have its uses and is the main way that doctors can test for gastro-intestinal infections and other bowel conditions like cancer. Lack of a sample can hinder diagnosis and so we need to encourage people to submit samples when they are asked to do so.
“We realise that most people find collecting poo an unpleasant thing to do. However there are ways that doctors can help patients to feel confident to fill the pot in the easiest way possible. Without guidance some people did actually think they had to just poo directly into the pot which adds to their distress. We want to encourage healthcare staff to take time to explain the importance of the sample in the patient’s treatment and to give our leaflet to help the collection process. Together these will help to increase the numbers of stool samples sent for testing which will help the patient’s care.”
The NHS Choices guide to collecting a stool sample.
Your GP or another healthcare professional such as a nurse should explain to you how to collect the stool sample. The stool sample should be collected in a clean, dry screw-top container. Your doctor or the hospital will provide you with a plastic (specimen) container to use, although you can use any clean container as long as you can seal it.
Try not to collect urine or water (from the toilet) with the stool sample but don’t worry if you do. If you need to urinate, do this first, and then collect the stool sample.
To collect a stool sample:
• label the container with your name, date of birth and the date
• place something in the toilet to catch the stool, such as a potty or an empty plastic food container, or spread clean newspaper or plastic wrap over the rim of the toilet
• make sure the sample doesn’t touch the inside of the toilet
• use the spoon or spatula that comes with the container to place the sample in a clean screw-top container and screw the lid shut
• if you’ve been given a container, aim to fill around a third of it (that’s about the size of a walnut if you’re using your own container)
• put anything you used to collect the sample in a plastic bag, tie it up and put it the bin
• wash your hands thoroughly with soap and warm running water
If your doctor gives you any other instructions, follow these also.
2. Bowel cancer screening consists of a home test kit known as a faecal occult blood (FOB) test. It works by detecting tiny amounts of blood which cannot normally be seen in poo. The FOB test does not diagnose bowel cancer, but the results will indicate whether further investigation (usually a colonoscopy) is needed. The risk of bowel cancer increases with age so it is important to return the sample if you are asked to give one by your doctor.
Bowel Cancer Awareness Month – April is Bowel Cancer Awareness Month – like and share to show your support
April is Bowel Cancer Awareness Month. To find out more information on Bowel Cancer Awareness Month you can check out the website for the month run by Bowel Cancer UK here http://www.bowelcanceruk.org.uk/month.
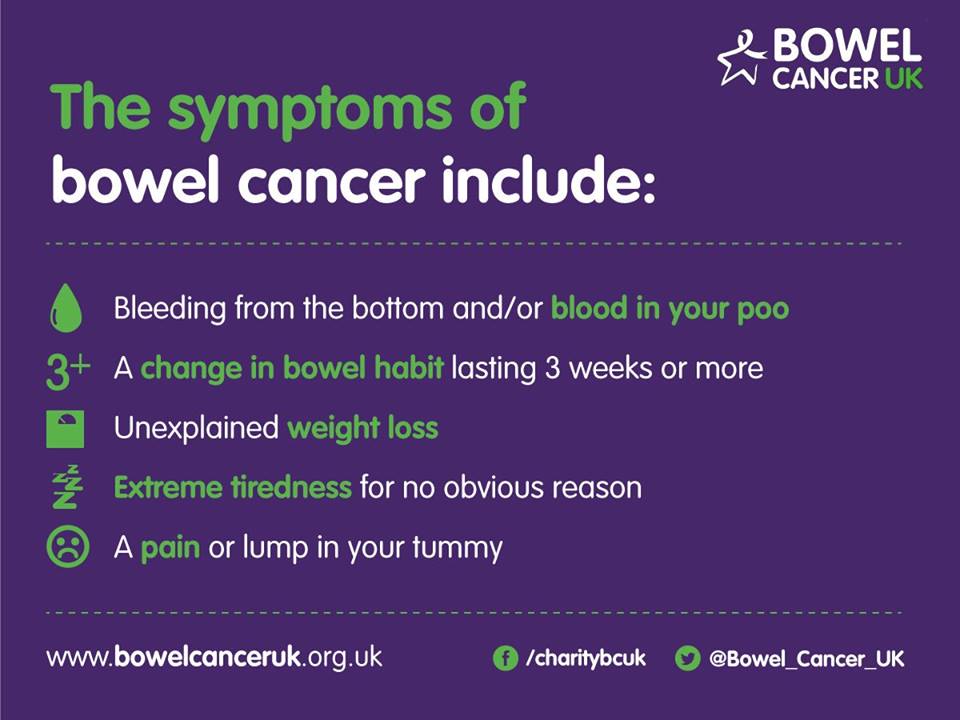
To show our support for the month we have produced the graphic below which we hope you will like and share with your friends and family.
Thanks very much in advance.
Concerns about young people and cancer being taken seriously says Bowel Cancer UK.
 Read our interview with Nick Bason of Bowel Cancer UK
Read our interview with Nick Bason of Bowel Cancer UK
A new report from Bowel Cancer UK makes suggests many younger bowel cancer patients have difficulty and delays in getting a bowel cancer diagnosis.
Bowel cancer is the second biggest cancer killer in the UK. Over 40,000 people are diagnosed each year and over 16,000 people will die from bowel cancer.
Bowel Cancer UK shares “Every year, over 2,100 people under the age of 50 are diagnosed with bowel cancer in the UK, a number which is growing. While this accounts for just 5% of people diagnosed with the disease in this country each year, the charity has released a report which shows that many younger people don’t feel they were or are being taken seriously by their GPs even if they come to them with bowel cancer symptoms as they are being perceived as too young.
Furthermore, a lack of information and education about the disease for people under 50, and a lack of clinical guidance from health authorities mean many younger people could be unaware that they are at risk of developing it.
National Institute for Health and Clinical Excellence (NICE) clinical guidelines, which apply in England and Wales, on referral for suspected lower gastrointestinal cancer, only covers people aged over 40 with specific symptoms, or people over 60 with more general symptoms.
There is no guidance for people under 40 and it’s a similar story in Scotland and Northern Ireland.
The ‘Never Too Young’ report released today which saw over 100 young bowel cancer patients surveyed found that 42% of women and 11% of men either saw their GP more than five times before being referred to a specialist, or were diagnosed as an emergency before being referred.
Almost a quarter of women and more than one in ten men had to wait over a year to get diagnosed, with Irritable Bowel Syndrome (IBS), haemorrhoids (piles) and anaemia the most common conditions to be diagnosed with before being correctly diagnosed with bowel cancer.
Prior to being diagnosed with bowel cancer, 90% of women were not aware that they could be at risk of bowel cancer, compared with 69% of men.
Close to 70% of men and 56% of women were not aware of the symptoms of bowel cancer prior to being diagnosed, while 91% of those surveyed think that there is a perception that bowel cancer only affects much older people.”
Alex Purkiss interviewed Nick Bason, Head of Policy and Public Affairs at Bowel Cancer UK on behalf of PatientTalk
BASON My name is Nick Bason, I am head of policy and public affairs at Bowel Cancer UK.
PURKISS Fabulous, thank you Nick. So to kick off then, how do you account for the rise of bowel cancer in young people?
BASON There has been a slow rise in the incidence of bowel cancer in young people over the last ten years but this is accompanied with a general rise in the number of people getting bowel cancer. In terms of the reasons, certainly diet and lifestyle do play a role in the development of bowel cancer, but particularly in younger people. It’s thought that there’s a particular genetic fault which is not fully understood yet that contributes to the development of bowel cancer in younger people.
PURKISS So this appears to be clearly a savage indictment of primary care in the UK. How should the clearly needed root and branch reform be carried out?
 BASON Well we don’t think it is a savage indictment of primary care in the UK. Our research found that delays in diagnosis, part of that is about delays I getting a referral from a GP to a diagnosis testing service, but also there are delays from a patient point of view as well with patients not going to the doctors until in some cases up to six months after they have developed symptoms. GPs play an important role in the diagnosis of bowel cancer of course and given the numbers of younger people affected by bowel cancer, most individual GPs will probably only see one or two people a year if that, so it can be quite hard to identify in younger people. And that’s why our report recommends better support and clinical guidance for GPs to help them refer younger people.
BASON Well we don’t think it is a savage indictment of primary care in the UK. Our research found that delays in diagnosis, part of that is about delays I getting a referral from a GP to a diagnosis testing service, but also there are delays from a patient point of view as well with patients not going to the doctors until in some cases up to six months after they have developed symptoms. GPs play an important role in the diagnosis of bowel cancer of course and given the numbers of younger people affected by bowel cancer, most individual GPs will probably only see one or two people a year if that, so it can be quite hard to identify in younger people. And that’s why our report recommends better support and clinical guidance for GPs to help them refer younger people.
PURKISS So how should younger folk be educated on this as well as other types of cancer?
BASON I think awareness campaigns that are run need to reflect the demographics of the disease. I think that a lot of the imagery that’s used about bowel cancer at the moment is around older people. So I think there’s the need to use younger people and recognise that bowel cancer is a condition that can affect younger people. Of course it is rare in younger people, but it can affect them so I think awareness campaigns need to reflect that imagery and in the messaging and in the channels that they use to get messages about bowel cancer awareness out through.
PURKISS And in terms of GPs, how can we best improve their training?
BASON We would like to see a bowel disease decision aid tool developed which can help GPs make decisions about younger people and which younger people to refer through for more testing and referred specialist services. I think that will help GPs when they are deciding who to refer and I think that needs to be supported by updating clinical guidance. Clinical guidance in the UK at the moment doesn’t cover people under 50 apart from in certain specific circumstances. And then I think GP training courses that are run by professional bodies really need to reflect the demographics of the disease and make sure the message is put across that although bowel cancer might be rare in younger people, it is potentially still an issue.
PURKISS So the health authorities have been targeted with strong criticism in particular. If you can detail perhaps how you think they might be to blame on this.
BASON Well again we don’t think that there is strong criticism of health authorities in our report. We think that they play an important role in ensuring that public health messages are disseminated to people in their areas, but we do say that health authorities and clinical commissioning groups really need to make sure that they are investing in the capacity in their endoscopy units locally, to make sure that their endoscopy units are supported to deal with the demand for testing. And I think that will then help GPs to refer people through and make sure people are tested and have access to those diagnostic services that they need.
PURKISS To go back to the study that was carried out, if you could give us a bit more of a breakdown in terms of how many people were interviewed, how they were conducted and a breakdown.
BASON So our research really focussed on, we spoke to a lot of younger people, we ran a focus group which was attended by ten younger people, we then ran a wider survey which was completed by over a hundred young people who were diagnosed with bowel cancer under the age of 50. We consulted with the Bowel Cancer UK medical advisory board and involved clinical experts in our report and we also conducted desk research as well.
PURKISS What would you say is the difference between the specific and relatively general symptoms?
BASON Well, part of the reason why bowel cancer is hard to diagnose is that a lot of the symptoms are also symptoms of other things. Extreme tiredness, a pain or lump in the tummy or weight loss can be symptoms of bowel cancer or they can be symptoms of other things. I think specifically to bowel cancer, a change in bowel habit which lasts for 3 weeks or more, blood in stools and bleeding from the bottom are specific symptoms of bowel cancer. I think that one of the points to make about symptoms with bowel cancer is that it’s the persistence of those symptoms. In our study we found one in four people were waiting over six months after developing symptoms before they went to the GP and clearly those people are living with some discomfort and pain and we would encourage younger people to go to the GP as soon as they develop symptoms.
PURKISS Just finally give us a bit more info there about where people can go to and what they need to do if they are concerned.
BASON Well if people are experiencing symptoms and they are concerned then we would encourage them to make an appointment at their local GP as soon as possible. If people want more information on the symptoms or the campaign then they can visit www.bowelcanceruk.org.uk and we also have a free, confidential advice service which people can ring up and details of that are on the website as well.
PURKISS Fabulous, good stuff, thank you very much
BASON Cheers