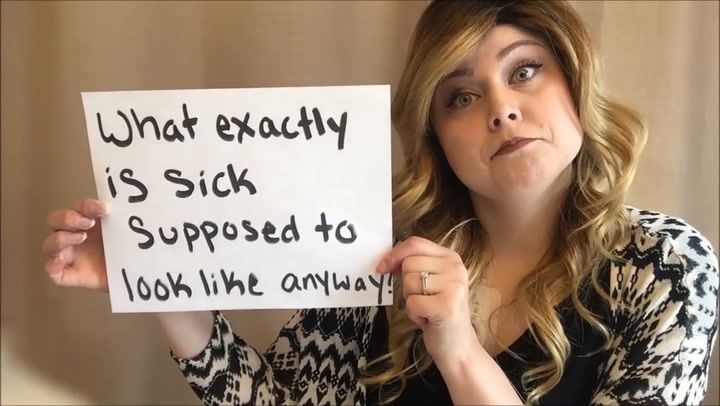
Just saw this brilliant video from Chanell white
The most frequent phrase many patients hear is, “but you don’t look sick!” I’ve heard it from family, friends, strangers, and even doctors! While that is a lovely compliment, I have always wondered what illness is supposed to look like for these individuals? The truth is illness often times is just hidden, only visible if you take a deeper look. It isn’t invisible like most people believe, it is just tucked away so the patient can live a more normal life. A coat of make-up and a cute outfit helps us feel more confident in our failing bodies, and seem more approachable to those around us.
Take to social media and post your side by side photos with the hashtag #invisibleorhidden
For more information on me, and my illness ‘Systemic Sclerosis’ visit my website at www.thetubefedwife.blogspot.com