On this video I explore some of the #autistic traits in adults that you may have never realised were signs of #autism. Plus, I share my personal lived experiences as an #actuallyautistic person.
On this video I explore some of the #autistic traits in adults that you may have never realised were signs of #autism. Plus, I share my personal lived experiences as an #actuallyautistic person.

Gabe is autistic and nonverbal. He has struggled with getting his haircut for most of his life. When we found his hairdresser Ping Gabe started to become more comfortable over time and with practice. Ping is also nonspeaking because she is deaf. In the past it would take several people to hold Gabe while he got his haircut and a lot of rewards. Now when he walks in he jumps into her chair on his own and allows her to give him a haircut. Recently he started to allow her to use the buzzer on him and style his hair with hair gel

ABC News’ Will Car reports on Sensory Cooking, a Phoenix-based organization tackling food aversions and sensitivity for children on the spectrum.

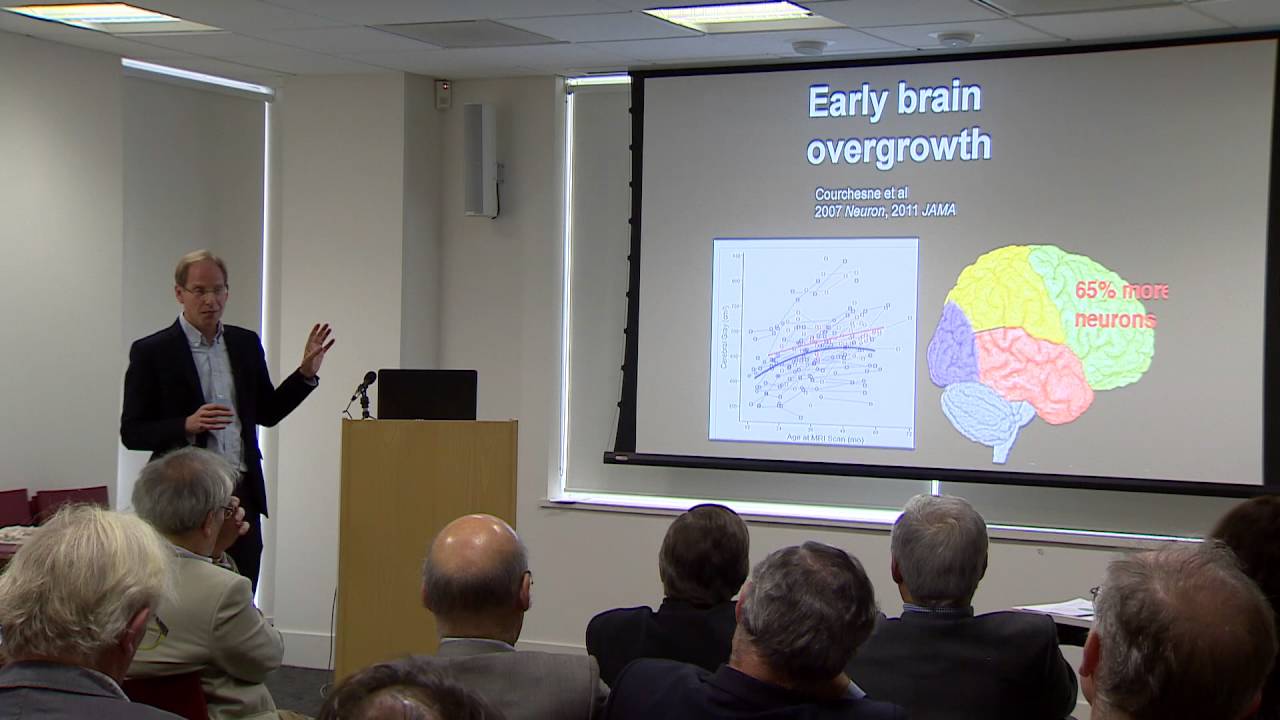
First Symposium of the Evolutionary Psychiatry Special Interest Group of the Royal College of Psychiatrists, Oct 4th 2016 in London. Lecture by Professor Simon Baron-Cohen from Cambridge University Autism Research Centre.