A new retrospective study with up to 40 years of follow-up shows significant reductions in death rates from all causes and cause-specific conditions such as cardiovascular disease, diabetes and cancer in patients who have undergone bariatric surgery compared to non-surgical participants with severe obesity, according to a new study in Obesity, The Obesity Society’s (TOS) flagship journal.
The study also found evidence suggesting an increased risk of death from chronic liver disease and higher death rates from suicide in younger patients who had bariatric surgery compared to non-surgical participants. The study’s authors observe that the findings of increased suicide rates among younger patients who have had bariatric surgery may promote more aggressive, pre-surgical psychological screening and post-surgery follow-up.
As a result of the decades-long durability of bariatric surgery in reducing death from all causes and decreasing deaths related to cardiovascular disease, diabetes and cancer compared to matched participants, researchers note the findings may not only increase interest in bariatric surgical treatment for patients with severe obesity but, in addition, further, stimulate necessary research related to the discovery of physiologic and biomolecular mechanisms leading to non-surgical treatment that results in weight loss and improved mortality similar to that achieved by bariatric surgery, said Ted D. Adams,
Experts explain that multiple association studies connecting bariatric surgery and mortality outcomes have been reported, predominantly retrospective, with wide variation in study design regarding participant number, control cohorts, mean follow-up, procedure type, age at surgery, clinical endpoints such as life expectancy and death rates for all causes and specific causes, and the presence or absence of prevalent diabetes. The new study builds upon the groups’ reported mortality outcomes following gastric bypass surgery by extending follow-up to 40 years, tripling the number of surgical patients, and using four, instead of one, bariatric surgery procedure.
Researchers used data from the Utah Population Database (UPDB) for the current study. The UPDB includes linked population-based information from Utah with statewide birth and death certificates, driver licenses and ID cards, and voter registration cards. The UPDB creates and maintains links between the database and the medical records held by Utah’s two largest healthcare providers.
Patients who had undergone bariatric surgery in Utah between 1982 and 2018 were identified from three, large bariatric surgical practices in Salt Lake City, Utah, and medical records from the University of Utah and Intermountain Healthcare Enterprise Data Warehouses in Salt Lake City. Non-surgical participants were selected from Utah driver’s license records or ID cards. Because driver’s licenses are generally renewed every five years, multiple records were available for selection to match the bariatric surgeries.
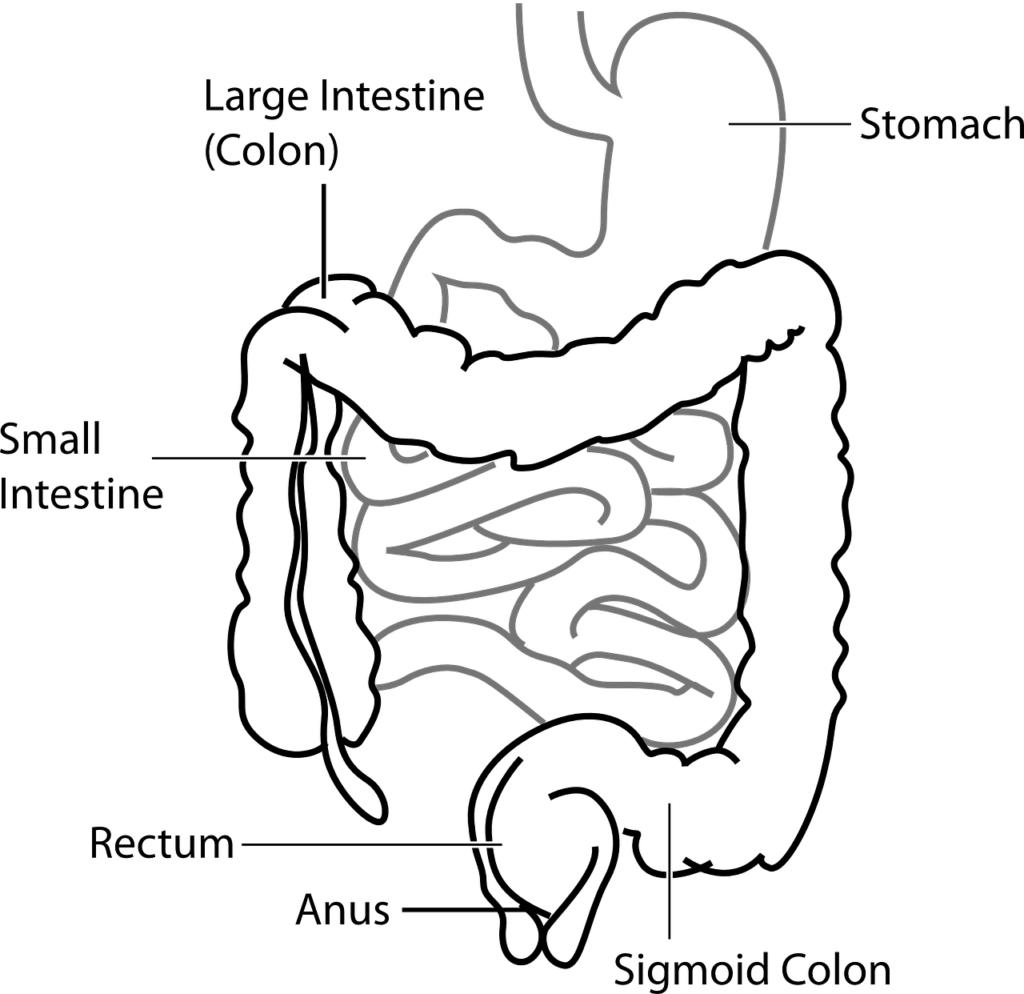
Nearly 22,000 participants with bariatric surgery and without were matched (1:1) for age, sex, body mass index and surgery date with a driver’s license/renewal date. Mortality rates were compared by Cox regression and stratified by sex, surgery type and age at surgery. Whereas mortality after gastric bypass surgery was previously reported from 1984 to 2002, this study extends mortality follow-up through 2021. The four bariatric surgery procedures included Roux-en-Y gastric bypass, adjustable gastric banding, sleeve gastrectomy and biliopancreatic diversion with a duodenal switch.
Results revealed that all-cause mortality was 16% lower in bariatric surgery patients than in non-surgical participants. Lower mortality was observed for both males and females. Mortality after surgery versus non-surgery decreased by 29%, 43% and 72% for cardiovascular disease, cancer and diabetes, respectively. Death rates for males and females from chronic liver disease were 83% higher in patients who had surgery than in non-surgical participants. The hazard ratio for suicide was 2.4 times higher in surgery compared with non-surgery participants, primarily in individuals with ages at the surgery between 18 and 34 years.
“This important study adds to the mounting evidence that bariatric surgery, not only improves the quality of life for patients but will also increase their life expectancy. This work will hopefully improve patients’ access to this effective treatment for obesity, which is still limited to only one per cent of qualified patients. Also, the study highlights the importance of providing more resources for pre-surgical psychological screening and post-surgery follow-up, especially for younger patients,” said Jihad Kudsi.