

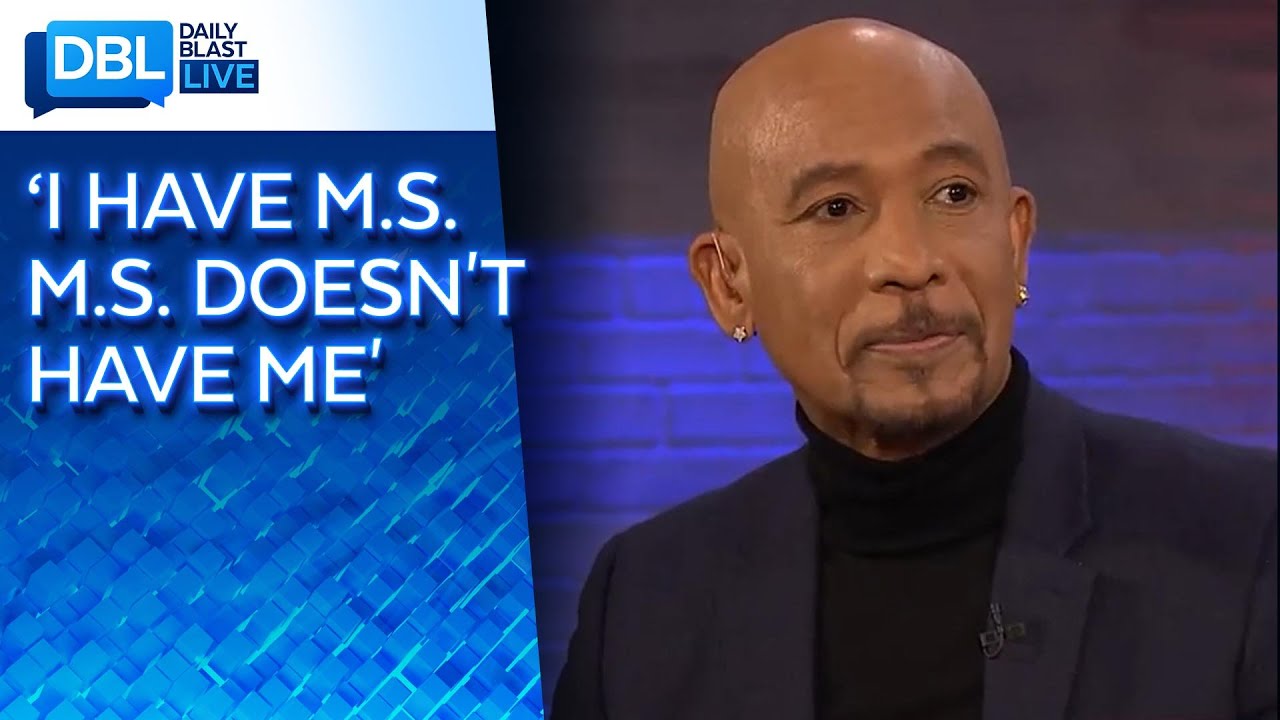
Montel Williams was diagnosed with Multiple Sclerosis, a disease with the highest rate of depression of any neurological disorder, in 1999. He opened up to us about his diagnosis, the conversations he’s had with Christina Applegate and Selma Blair, and how he’s doing now with a new experimental protocol. Montel also shares info about a treatment that he says is one of the only cures for PTSD, called Reconsolidation of traumatic memories (RTM). He tells us more about it and what it can do for veterans.
An fMRI scan of the brain of a military veteran with PTSD, showing gray matter regions with increased myelin CREDIT UCSF image by Linda Chao
A recent study links anxiety behavior in rats, as well as post traumatic stress disorder (PTSD) in military veterans, to increased myelin — a substance that expedites communication between neurons — in areas of the brain associated with emotions and memory.
The results, reported by scientists at the University of California, Berkeley, and UC San Francisco (UCSF), provide a possible explanation for why some people are resilient and others vulnerable to traumatic stress, and for the varied symptoms — avoidance behavior, anxiety and fear, for example — triggered by the memory of such stress.
If, as the researchers suspect, extreme trauma causes the increased myelination, the findings could lead to treatments — drugs or behavioral interventions — that prevent or reverse the myelin production and lessen the aftereffects of extreme trauma.
Myelin is a layer of fatty substances and proteins that wraps around the axons of neurons — essentially, the insulation around the brain’s wiring — to facilitate long-distance transmission of signals and, thus, communication between distant areas of the brain. The inner regions of the brain look white — in fact, they are referred to as “white matter” — because of the myelin encasing the many large bundles of axons there.
But the new study finds increased myelination of axons in so-called “gray matter,” where most of the cell bodies of neurons reside and most of the wiring is less insulated with myelin. The extra myelination was found primarily in areas associated with memory.
Researchers at the San Francisco Veterans Affairs Medical Center conducted brain MRI scans of 38 veterans — half with PTSD, half without — and found an increase in myelination in the gray matter of those with PTSD compared to that seen in the brains of those not suffering from PTSD.
Colleagues at UC Berkeley, meanwhile, discovered a similar increase in myelination in the gray matter of adult rats subjected to an acute stressful event. While not all rats showed long-term effects from the stress — just as not all traumatized veterans develop PTSD — those that did had increased myelination in specific areas of the brain associated with particular symptoms of stress that was identical to what UCSF physicians found in veterans with PTSD.
Both veterans with PTSD and stressed rats that exhibited avoidance behavior, for example, had increased myelination in the hippocampus, often thought of as the seat of memory. Those exhibiting a fear response had increased myelination in the amygdala, which plays a key role in our response to strong emotions, such as fear or pleasure. Those suffering from anxiety had increased myelination in the dentate gyrus, a region critical to learning and memory.
“The combination of these studies in rats with our population of veterans with post traumatic stress disorders is, to me, really exciting,” said senior author Dr. Thomas Neylan, director of the Posttraumatic Stress Disorders (PTSD) Clinic and the Stress and Health Research Program at the San Francisco VA. “At least it’s another mechanism to think about as we develop new treatments. If we see enduring ability to shape myelin content in an adult brain, maybe treatments will help reverse this. That’s where we want to go next with this.”
People — and rats — vary in their response to stress
The correlation between the symptoms and the region of myelination was discovered because UC Berkeley researchers subjected the rats to a battery of more than a dozen tests to assess their specific behavioral response to acute stress.
“We understand that there’s a lot of individual variation in humans, but with rats, they’re genetically identical, so you think when you expose them to stress you’re going to get the same response,” said senior author Daniela Kaufer, UC Berkeley professor of integrative biology. “But the response is extremely variable. They sort of fall into groups, such that some are really resilient, and some are vulnerable. And the ones that are vulnerable are vulnerable in different ways: Some show avoidance behavior, and some show fear learning problems, and some show startle responses that are exaggerated.”
According to Neylan, similar individuality is seen in people with PTSD. The new study suggests that the specific symptoms are related to which areas of the brain are being newly myelinated.
“There’s a lot of heterogeneity across different people with PTSD; it’s not one size fits all. Every PTSD patient generally has a mix of different symptoms,” said Neylan, professor-in-residence in psychiatry at the UC San Francisco Weill Institute for Neurosciences. “Some people are very avoidant. Some people are very hyperreactive. The idea is that if you can show that these different symptom clusters have different neural circuitry, it might actually lead us closer to subtyping people in a way that we could be more targeted in our treatment.”
The researchers, who published their results in December 2021 in the journal Translational Psychiatry, show that stress produces more of the brain’s glial cells, called oligodendrocytes, which wrap around the axons of neurons and make the myelin. The increased myelin produced by these new oligodendrocytes could affect the speed of connections between neurons, making some connections hyperresponsive.
“In the gray matter of your cortex, most of the dendrites and axons — the projections that come out of the neurons that help establish communications with other neurons — can form thousands of connections, and most of them are unmyelinated,” Neylan said. “But if experience leads you to start to lay down myelin to strengthen certain connections, let’s say your ability to respond quickly to a fearful stimulus, you can speed up that circuit, but you lose the kind of broader adaptive flexibility that you normally would have with mostly unmyelinated axons and dendrites. People with PTSD become almost like a one-note musician — they really know how to respond to fear. But that enhanced, quick response to fear may diminish their adaptive flexibility for non-fear-type behavior.”
Acute stress boosts oligodendrocytes
In 2014, Kaufer and her UC Berkeley colleagues discovered that rats subjected to acute stress produced more oligodendrocytes in the brain’s gray matter — specifically, in the hippocampus. She proposed that this led to increased myelination of axons, potentially interfering with the speed at which signals traveled between different areas of the gray matter of the brain, such as the hippocampus and the amygdala. The new study bolsters that theory.
Neylan was intrigued by the 2014 findings and contacted Kaufer, and they’ve been collaborating ever since. Neylan teamed up with Linda Chao, UCSF professor of radiology, who developed a way to image myelin in the gray matter of the brain, and several years ago scanned the brains of 38 veterans who had experienced severe trauma, some with and some without PTSD.
At the time, scientists looking for changes in myelination related to brain disorders were focused on the cortex’s white matter, which is mostly myelinated. In multiple sclerosis, for example, an autoimmune attack destroys myelin in the white matter. Kaufer was perhaps the first to find evidence of increased myelination in the gray matter associated with disease.
Chao and Neylan did find increased myelination of neurons in the gray matter of veterans with PTSD, but not in those without PTSD. The worse the symptoms, the greater the myelination.
This led Kaufer and first author Kimberly Long, now a UCSF postdoctoral fellow, to see if they could also find increased myelin in gray matter after acute trauma in rats. After they focused on the specific symptoms of individual rats with PTSD, they found a correlation between symptoms and myelination in specific regions of the gray matter.
Chao subsequently reanalyzed the brain scans of her earlier group of 38 veterans and found the same correlation: Specific symptoms were associated with myelination in one region of gray matter, but not others.
Long and Kaufer then employed a type of viral gene therapy to rev up a transcription factor, called olig1, that increases the production of oligodendrocytes from stem cells in the gray matter. When Long injected the virus into the dentate gyrus of rats, the researchers found that this boosted the number of oligodendrocytes and generated symptoms of avoidance, even without any stress.
“The next question was, ‘If I change oligodendrocyte genesis, am I going to change behavior?” Kaufer said. “The beginning of an answer is here in this paper — it’s yes. And now, there’s a lot more to do to really understand that.”
Neylan, Chao and Kaufer are collaborating on further studies, including looking for increased myelin in the brains of PTSD patients who have died, improving fMRI imaging of myelin in the brain, investigating the effects of chronic stress on the brain connections of rats, and using new high-resolution imaging to study the myelin deposition in gray matter.
The work was supported by a grant from National Institute of Mental Health of the National Institutes of Health (R01MH115020).
Other co-authors of the paper were undergraduates Yurika Kazama, Vivian Roan, Rhea Misra, Anjile An, Kelsey Hu, and Claire Toth and doctoral student Jocelyn Breton of UC Berkeley; UCLA undergraduate Lior Peretz; University of Arizona undergraduate Dyana Muller; University of British Columbia (UBC) doctoral student William Casazza; UBC professor Sara Mostafavi; Boston University neurologist Dr. Bertrand Huber; and researcher Steven Woodward of the VA Palo Alto Health Care System.

The symptoms of autism trauma and PTSD (post traumatic stress disorder) can look very similar. So what’s the overlap? And how are they different? Can childhood trauma cause autism? (Hint: No, there’s a very important distinction) In this video we’ll explore complex trauma and how the polyvagal theory and principles of trauma informed care can help improve autistic mental health.
Someone with PTSD often relives the traumatic event through nightmares and flashbacks, and may experience feelings of isolation, irritability and guilt.
They may also have problems sleeping, such as insomnia, and find concentrating difficult.
These symptoms are often severe and persistent enough to have a significant impact on the person’s day-to-day life.
Read more about the symptoms of PTSD.
The type of events that can cause PTSD include:
serious road accidents
violent personal assaults, such as sexual assault, mugging or robbery
prolonged sexual abuse, violence or severe neglect
witnessing violent deaths
military combat
being held hostage
terrorist attacks
natural disasters, such as severe floods, earthquakes or tsunamis
PTSD can develop immediately after someone experiences a disturbing event or it can occur weeks, months or even years later.
PTSD is estimated to affect about 1 in every 3 people who have a traumatic experience, but it’s not clear exactly why some people develop the condition and others don’t.
Read more about the causes of PTSD.
People who repeatedly experience traumatic situations such as severe neglect, abuse or violence may be diagnosed with complex PTSD.
Complex PTSD can cause similar symptoms to PTSD and may not develop until years after the event. It’s often more severe if the trauma was experienced early in life as this can affect a child’s development.
Read more about complex PTSD.
It’s normal to experience upsetting and confusing thoughts after a traumatic event, but most people improve naturally over a few weeks.
You should visit your GP if you or your child are still having problems about four weeks after the traumatic experience, or if the symptoms are particularly troublesome.
If necessary, your GP can refer you to mental health specialists for further assessment and treatment.
PTSD can be successfully treated, even when it develops many years after a traumatic event.
Any treatment depends on the severity of symptoms and how soon they occur after the traumatic event. Any of the following treatment options may be recommended:
Watchful waiting – monitoring your symptoms to see whether they improve or get worse without treatment.
Antidepressants – such as paroxetine or mirtazapine.
Psychological therapies – such as trauma-focused cognitive behavioural therapy (CBT) or eye movement desensitisation and reprocessing (EMDR). You can refer yourself directly to a psychological therapies service.
Find a psychological therapies service in your area.
Read more about treating PTSD.
Cases of PTSD were first documented during the First World War when soldiers developed shell shock as a result of the harrowing conditions in the trenches.
But the condition wasn’t officially recognised as a mental health condition until 1980, when it was included in the Diagnostic and Statistical Manual of Mental Disorders, developed by the American Psychiatric Association.