The results of a pilot study presented today at the Annual European Congress of Rheumatology (EULAR 2019) suggest that electro stimulation of one of the nerves connecting the brain to the body (the vagus nerve), could provide a novel treatment approach for patients with rheumatoid arthritis.1
“This is a really exciting development. For many patients suffering from rheumatoid arthritis, current treatments don’t work, or aren’t tolerated,” said Professor Thomas Dörner, Chairperson of the Scientific Programme Committee, EULAR. “These results open the door to a novel approach to treating not only rheumatoid arthritis, but other chronic inflammatory diseases. This is certainly an area for further study.”
The vagus nerve is the longest and the most complex of the 12 pairs of cranial nerves that originate from the brain. The name ‘vagus’ comes from the latin word for ‘wandering’. This is because the vagus nerve wanders from the brain into the organs of the neck, chest and abdomen.
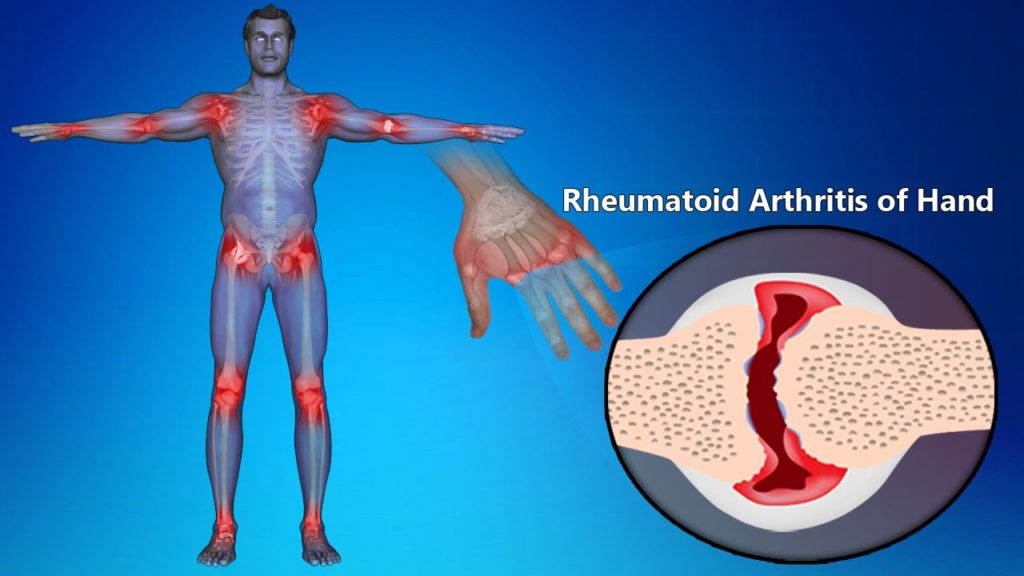
Recent advances in neuroscience and immunology have mapped circuits in the brain that regulate immune responses. In one of the circuits, the ‘inflammatory reflex’, signals are transmitted in the vagus nerve that inhibit the production of cytokines including tumor necrosis factor (TNF), an inflammatory molecule that is a major therapeutic target in rheumatoid arthritis. It is thought that, by stimulating the activity of this inflammatory reflex, innate immune responses can be modulated without abolishing them or producing significant immunosuppression.
In this pilot study, a novel miniaturised neurostimulator called a MicroRegulator was implanted into 14 patients with rheumatoid arthritis who had failed on at least two biologics or targeted oral therapies with different mechanisms of action. Patients were randomised to three groups who were either placebo, stimulated once daily, or stimulated four times a day for 12 weeks. At the end of the study, the patients who received once-daily stimulation were shown to have a better response than those on four-times-daily stimulation with two thirds meeting the EULAR good or moderate response criteria and a mean change in DAS28-CRP of -1.24. The mean change in DAS28-CRP* in the placebo group was 0.16.1
Cytokines (a broad and loose category of small proteins that are important in cell signalling) were also measured in the study with the actively stimulated groups showing a decrease of more than 30% in levels of Interleukin (IL) 1β, IL-6, and TNF-α. Implantation and stimulation were generally well tolerated with no device or treatment-related SAEs and two surgery-related adverse events that resolved without clinically significant effects.1
“Our pilot study suggests this novel MicroRegulator device is well tolerated and reduces signs and symptoms of rheumatoid arthritis,” said Mark Genovese, M.D., James W. Raitt Endowed Professor of Medicine, Stanford University, Stanford, California, USA. “These data support the study of this device in a larger placebo-controlled study as a novel treatment approach for rheumatoid arthritis and possibly other chronic inflammatory diseases.”
This study follows a proof-of-concept study which used reprogrammed epilepsy stimulators on the vagus nerve to demonstrate reduced systemic inflammation and improved disease activity in 17 patients with rheumatoid arthritis.3
The study included 14 patients with active rheumatoid arthritis who had had an insufficient response to more than two biological disease modifying anti-rheumatic drugs (bDMARDs) or JAK inhibitors with more than two modes of action. All patients remained on stable background of methotrexate. The first three patients were implanted and stimulated after three weeks, following safety review board approval, the remaining 11 patients were implanted and randomised to one minute of stimulation once-daily, one minute of stimulation four times daily, or one minute of placebo stimulation.1