A current Swedish study came to the result that among patients with high disease activity, one in one hundred will develop venous thromboembolism within one year, a more than twofold increase compared to patients in remission (1). Data of the German RABBIT1 register (2) published by the European League against Rheumatism (EULAR) show that this increased risk of thrombosis can be reduced by treatment with biological disease-modifying antirheutmatic drugs (bDMARD). This is important information, especially at this time during the COVID-19 pandemic, since thrombosis and pulmonary embolism also play a major role in COVID-19 infection. Vigilance for thrombosis during the treatment of people with arthritis is particularly recommended. Moreover, maintaining therapies to keep disease activity under control is vital.
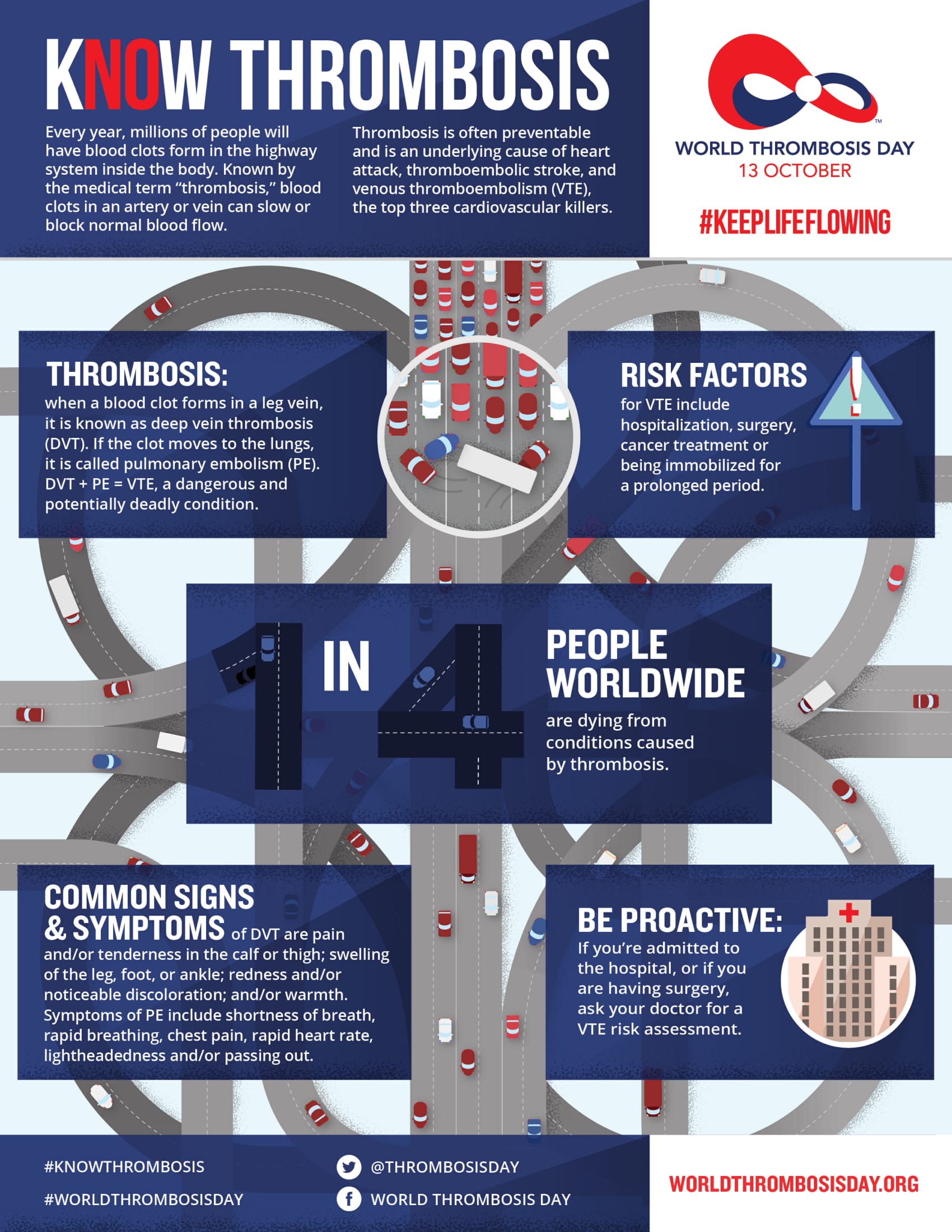
Thrombosis is a significant medical problem. In the case of venous thromboembolism (VTE), clotting occurs inside a blood vessel and can affect the blood flow. Quick diagnosis and treatment are important as untreated deep vein thrombosis (DVT) in the leg can lead to potentially life-threatening pulmonary embolism: Parts of the thrombus tear off and enter a pulmonary vessel through the blood stream. In up to 30 percent of cases, patients die within 30 days after diagnosis from deep vein thrombosis in the leg or pulmonary embolism (3).
Due to chronic inflammation in patients suffering from rheumatoid arthritis, the risk of dangerous deep vein and pulmonary thrombosis is two to three times as high (3). “In the case of autoimmune diseases such as rheumatoid arthritis (RA), the immune system turns against the body and causes inflammation in a number of places. Inflammation may have a disruptive effect on coagulation,” explains EULAR President Professor Dr. med. Iain B. McInnes from The University of Glasgow, UK. In people who are suffering from rheumatoid arthritis, the risk of thrombosis must always be taken into account.
The factors promoting thrombosis in patients suffering from rheumatoid arthritis and the medication that potentially reduces the risk have now been examined in two current studies.
One in one hundred patients with RA increased disease activity will suffer from thrombosis:
A Swedish cohort study tried to find an answer to the question of whether the degree of disease activity has an impact on the thrombosis risk (1). The team around Viktor Molander, PhD student at the Karolinska Institutet in Stockholm analysed the data of 46,311 patients suffering from RA taken from the Swedish Rheumatology Quality Register (SRQ) over a period of 12 years. For the measurement of disease activity the “Disease Activity Score 28” (DAS28) was used. The DAS28 assesses the disease activity of rheumatoid arthritis based on the assessment of 28 defined joints.
The study indicates a close connection between the clinical disease activity of RA measured by DAS28 and the risk of VTE: Molander came to the result that “among patients with high disease activity, one in one hundred is going to develop VTE within the following year, a more than twofold increase compared to patients in remission.”
“Having regular check-ups by a rheumatologist can be inconvenient. However, it is an important measure to monitor the development of the condition and whether treatment has to be adjusted accordingly,” explains EULAR Scientific Chair Professor Dr. John Isaacs from The University of Newcastle, UK.
Biologics can reduce the risk of thrombosis:
The risk of thrombosis is also influenced by the medication used in rheumatoid arthritis cases. Conventional synthetic disease-modifying anti-rheumatic drugs (csDMARD) such as Methotrexate, Sulfasalazine and Leflunomide are part of the basic treatment of RA. A next step are biologics (bDMARD), which also include tumour necrosis factor (TNF) inhibitors like Adalimumab, Certolizumab Pegol, Etanercept, Golimumab and Infliximab.
The question of whether the risk of thrombosis is reduced by application of bDMARDs such as TNF inhibitors in comparison to csDMARDs was addressed in a scientific study including the lead author Dr. rer. nat. Martin Schäfer from the programme area of Epidemiology at the German Rheumatism Research Center, Berlin, Germany. For this purpose, the team has analysed the data of more than 11,000 RA patients in the German RABBIT1 register, who were treated either with another csDMARD after at least one csDMARD failure, or whose treatment was switched to bDMARD.
The result: “By treatment with TNF inhibitors, the risk of major VTE events is reduced by almost half in comparison to csDMARDs,” explains Schäfer. According to the RABBIT data, an increase in inflammatory activity was also associated with a significant increase in the risk of VTE: The risk was approximately twice as high as a CRP value of at least 5 mg/l. “For patients with an increased risk of thrombosis, alternative treatment with TNF inhibitors, and possibly other biologic drugs, should be considered instead of standard csDMARD treatment,” concludes PD Dr. med. Anja Strangfeld, study manager at RABBIT register in Berlin and co-author of the study. “Reducing the inflammatory activity is also an important factor to reduce the risk of VTE.”