MMJ and MS
Oral spray containing two compounds derived from the cannabis plant reduced spasticity compared with placebo in patients already taking anti-spasticity drugs.
Chemical compounds derived from the cannabis sativa plant given as an add-on treatment may help ease symptoms of spasticity (tight or stiff muscles), a major cause of disability and reduced quality of life in people with motor neuron disease, according to a phase 2 trial of 60 adults published in The Lancet Neurology journal.
The findings show for the first time that adults with motor neuron disease taking first-line anti-spasticity drugs who were then treated with an oral spray (nabiximols) containing equal parts delta-9 tetrahydrocannabinol THC and cannabidiol (THC-CBD) experienced less spasticity and pain at 6-week follow-up compared with those given placebo.
While there are several drugs to relieve spasticity, evidence for their effectiveness is scant and they do not sufficiently improve symptoms in all patients. Moreover, they can have undesirable side effects, such as increasing muscle weakness and fatigue. In the study, participants continued taking other medications throughout the trial.
“There is no cure for motor neuron disease, so improved symptom control and quality of life are important for patients,” says Dr Nilo Riva from the San Raffaele Scientific Institute in Milan, Italy, who led the research. “Our proof-of-concept trial showed a beneficial effect of THC-CBD spray in people on treatment-resistant spasticity and pain. Despite these encouraging findings, we must first confirm that THC-CBD spray is effective and safe in larger, longer term phase 3 trials.” [1]
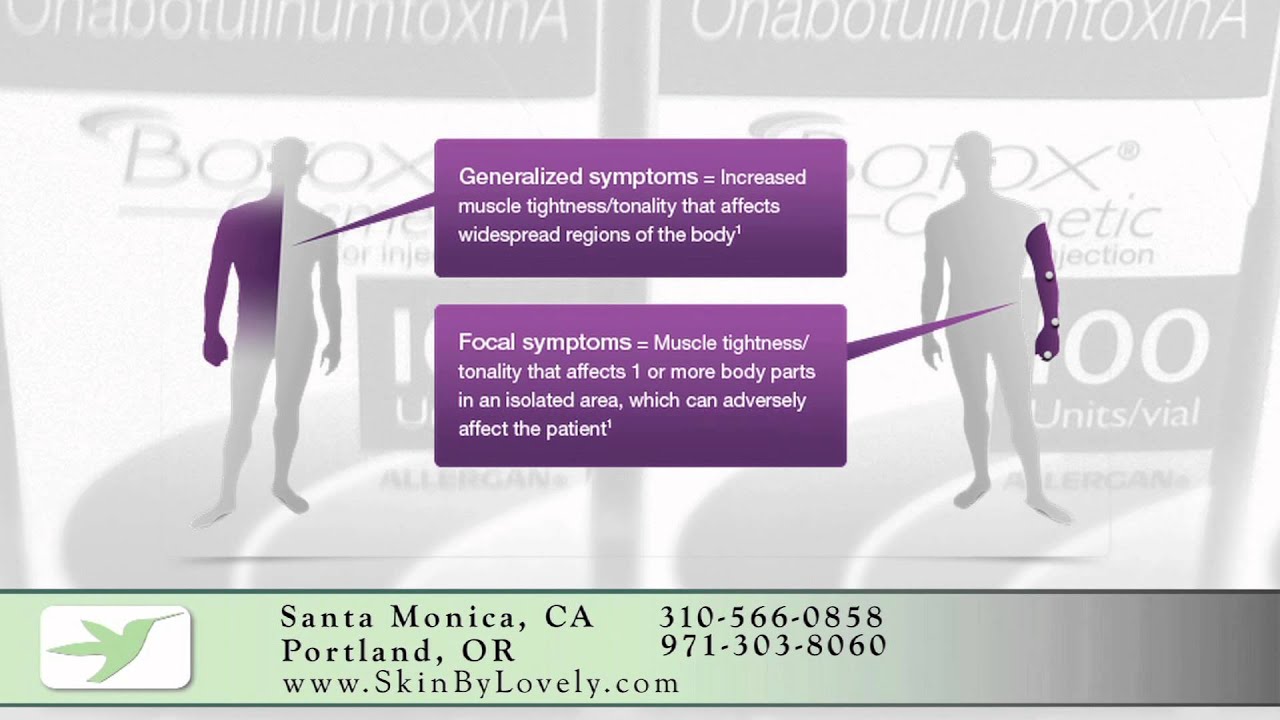
Spasticity is a common symptom in motor neuron disease, a rapidly progressive, fatal neurodegenerative disorder affecting the nerve cells that control muscle movement (motor neurons). It occurs to a variable degree in people with amyotrophic lateral sclerosis (ALS), the most common and severe form of motor neuron disease, and is a defining characteristic of primary lateral sclerosis (PLS), that is rarer and progresses more slowly.
Previous research has found possible therapeutic benefits of cannabinoids (components of the cannabis plant) to include muscle relaxation, appetite stimulation, and pain-relieving, anticonvulsant, and anti-inflammatory effects in patients with other neurological conditions. Cannabinoids have been licensed in several countries for symptomatic treatment of spasticity in multiple sclerosis, and are increasingly recognised as a valuable option for the management of pain.
To investigate whether cannabinoids might also reduce spasticity in motor neuron disease, Italian researchers recruited 60 adults (aged 18-80 years) with ALS or PLS from four tertiary motor neuron disease centres in Italy. To participate in the study, patients had to have experienced spasticity symptoms for at least 3 months and be taking a stable dose of any anti-spasticity medication for 30 days before enrolment and throughout the study.
Participants were randomised to receive THC-CBD mouth spray (29 participants) or placebo (30) for 6 weeks. The number of sprays was gradually increased for the first 2 weeks of treatment until the optimum dose was reached, and then that dose was maintained for 4 weeks.
Change in spasticity was assessed by a physician who rated the spasticity of each participant’s joints on the Modified Ashworth Scale (MAS)–an objective tool to evaluate intensity of muscle tone. Participants were also asked to keep a daily symptom diary on spasticity levels, pain, spasm frequency, and sleep disruption.
At the end of treatment (6 weeks), spasticity was significantly improved in the THC-CBD spray group compared with the placebo group (mean MAS-scores improved by an average 0.11 vs deteriorated by an average 0.16). Additionally, the number of participants treated with THC-CBD spray reporting an improvement was significantly higher compared with participants receiving placebo (55%; 16/29 participants vs 13%; 4/30). Finally, pain scores were significantly improved in the THC-CBD spray group compared with placebo on a 0-10 scale (-0.97 vs -0.06).
Overall, THC-CBD spray was well tolerated and adverse events were mild to moderate and typical of cannabinoids–asthenia (loss of energy and fatigue), somnolence (sleepiness), vertigo, and nausea. Twenty-one (72%) participants in the THC-CBD spray group and four (13%) in the placebo group reported at least one potentially treatment-related adverse event. There were no serious adverse events and no participants permanently discontinued treatment. However, three patients temporarily discontinued treatment in the THC-CBD spray group, two because of adverse events (one had nausea and anxiety and the other influenza), and one because of disease progression.
The authors note that an important limitation of the study was that the Modified Ashworth Scale has lacked sensitivity in studies assessing cannabinoids efficacy in multiple-sclerosis-related spasticity.
Writing in a linked Comment, Dr Marinne de Visser from Amsterdam University Medical Centre, University of Amsterdam, the Netherlands, says: “Before asking for approval of cannabinoids for symptomatic treatment of spasticity in patients with amyotrophic lateral sclerosis, further studies are needed to establish the frequency of spasticity in the various presentations of motor neuron disease, and also whether reductions in spasticity improve quality of life. Natural history studies including all subtypes of motor neuron disease and better outcome measures aimed at assessment of spasticity are required. Riva and colleagues’ data are encouraging, and larger multicentre randomised controlled trials should be done to identify which subgroups of patients derive clinically significant benefits from nabiximols.”