For the first time, researchers at the UNC School of Medicine showed they could target one brain region with a weak alternating current of electricity, enhance the naturally occurring brain rhythms of that region, and significantly decrease symptoms associated with chronic lower back pain.
The results, published in the Journal of Pain and presented at the Society for Neuroscience conference in San Diego this week, suggest that doctors could one day target parts of the brain with new noninvasive treatment strategies, such as transcranial alternating current stimulation, or tACS, which researchers used in this study to boost the naturally occurring brain waves they theorized were important for the treatment of chronic pain.
“We’ve published numerous brain stimulation papers over several years, and we always learn something important,” said senior author Flavio Frohlich, PhD, director of the Carolina Center for Neurostimulation and associate professor of psychiatry. “But this is the first time we’ve studied chronic pain, and this is the only time all three elements of a study lined up perfectly. We successfully targeted a specific brain region, we enhanced or restored that region’s activity, and we correlated that enhancement with a significant decrease in symptoms.”
Co-first author Julianna Prim, a graduate student mentored by Karen McCulloch, PT, PhD, in the Department of Allied Health Sciences at the UNC School of Medicine, who works closely with Frohlich’s lab, said, “If brain stimulation can help people with chronic pain, it would be a cheap, non-invasive therapy that could reduce the burden of opioids, which we all know can have severe side effects.”
Chronic pain is the leading cause of disability in the world, but there is not consensus among scientists that brain activity plays a causal role in the condition. Frohlich says the pain research field has focused largely on peripheral causes of chronic pain. For example, if you have chronic lower back pain, then the cause and solution lie in the lower back and related parts of the nervous system in the spine. But some researchers and clinicians believe chronic pain runs deeper, that the condition can reorganize how cells in the nervous system communicate with each other, including networks of neurons in the brain. Over time, the theory goes, these networks get stuck in a kind of neural rut, essentially becoming a cause of chronic pain.
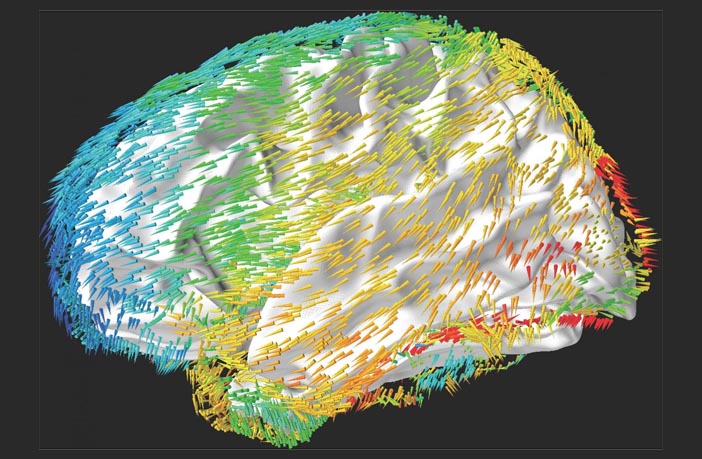
Previous studies showed that people with chronic pain experience abnormal neural oscillations, or brain waves. There are several kinds of brain waves related to different brain regions and various kinds of brain activities – processing visual stimuli, memorization, creative thinking, etc. When we speak, think, eat, play sports, watch television, daydream, or sleep, our brain activity creates electrical patterns researchers can measure using electroencephalograms, or EEGs. These patterns fluctuate or oscillate, which is why they appear as waves that rise and fall on an EEG printout.
One type of brain activity is called alpha oscillations, which occur when we are not taking in stimuli. When we meditate in silence, daydream in the shower, or even when we’re “in the zone” during athletic activity, alpha oscillations dominate the brain. Frohlich’s lab wanted to know if these alpha oscillations were deficient in the somatosensory cortex, located in the middle portion of the brain and likely involved in chronic pain. If so, then could Frohlich’s team enhance the alpha waves there? And if that were possible, would there be any pain relief?
Prim and colleagues recruited 20 patients with lower chronic back pain. Each of them reported back pain as “four” or greater for at least six months on the subjective scale of one to 10. Each participant volunteered for two 40-minute sessions that took place one to three weeks apart.
During all sessions, researchers attached an array of electrodes to the scalps of patients. During one session, researchers targeted the somatosensory cortex using tACS to enhance the naturally occurring alpha waves. During another session for all participants, researchers used a similar weak electrical current that was not targeted – this was a sham or placebo stimulation session. During all sessions, participants felt tingling on their scalp. They could not tell the difference between the sham and tACS sessions. Also, the researchers in charge of analyzing the data did not know when each participant underwent the sham or tACS sessions, making this study double-blinded.
Co-first author Sangtae Ahn, PhD, a postdoc in Frohlich’s lab, analyzed the data, which showed that Frohlich’s team could indeed successfully target and enhance alpha oscillations in the somatosensory cortex of people with chronic lower back pain. When Prim and colleagues surveyed the participants, all of them reported a significant reduction in pain immediately following the tACS sessions, according to the subjective 0-10 pain scale. Remarkably, some participants reported feeling no pain after the tACS sessions. Participants did not report the same pain reduction after the sham stimulation sessions.
“The exciting thing is that these results occurred after just one session,” Prim said. “We hope to conduct a larger study to discover the effects of multiple tACS sessions over a longer time period.”
Frohlich said his lab also hopes to conduct studies on people with various kinds of chronic pain.
“This study is a perfect example of what’s possible when scientists and clinicians collaborate,” he said. “Ultimately, if we want to develop better treatments, cures, and prevention strategies, then these sorts of new approaches that bring researchers together are of fundamental importance.”