A recent study of more than 2,700 older Canadians reported older adults with diabetes faced a heightened risk of depression during the COVID-19 pandemic. In this cohort, almost 50% of those who had a pre-pandemic history of depression experienced depression during the pandemic.
Those who experienced loneliness were among the most impacted.
“During the pandemic, loneliness almost tripled the risk of depression in older adults with diabetes,” says clinical pharmacist and first author ZhiDi Deng. “This not only highlights the impact of quarantines and lock-downs on individuals’ mental health. It also shows us that there is room for improvement on how we can better deliver services to older adults with diabetes in future public health crises.”
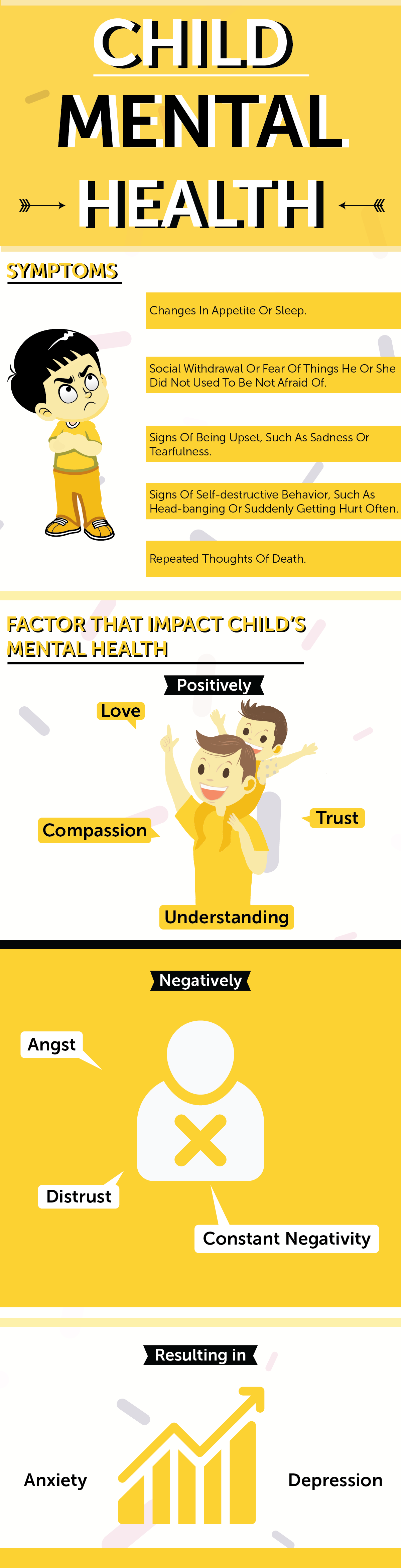
Although not as severely impacted as those with a history of depression, one in eight older adults with diabetes who had no history of depression prior to the pandemic were depressed in the autumn of 2020. “The pandemic has taken a significant toll on the mental health of everyone, particularly older adults with chronic conditions such as diabetes,” says co-author Grace Li, a research assistant at the University of Toronto’s Institute for Life Course and Aging (ILCA). “It’s important for primary health providers to be vigilant for signs of depression among their older patients, even those who were doing well in the past.”
The researchers identified several other factors that were associated with a higher risk of depression among those with diabetes, such as being female, having functional limitations or chronic pain, and experiencing family conflict.
They also reported some unexpected findings. The researchers found that those who were separated, divorced, or widowed had lower odds of recurrent depression during the pandemic than those who were married or in common-law relationships. “This is different from research conducted before the pandemic that indicated married individuals usually are less depressed,” said co-author Dorina Cadar, Senior Lecturer in Neuroepidemiology and Dementia at the Centre for Dementia Studies at Brighton and Sussex Medical School and the director of the Cognitive Epidemiology, Dementia, and Ageing Research lab. “We hypothesized that participants who were married during the pandemic experienced worse mental health because the need to stay for extended periods of time in close living proximity during the lockdowns or quarantine could possibly exacerbate any relationship conflicts. Our findings indicate that those who were experiencing family conflict during the pandemic had more than triple the risk of depression during the pandemic.”
The second unexpected finding was that those with higher income prior to the pandemic had a greater risk of depression during the pandemic than those who were poorer. In pre-pandemic research, higher income is associated with a lower prevalence of depression.
“We hypothesized that this finding may have been influenced by the generous response of the Canadian government with the Canadian Emergency Response Benefit (CERB), which may have had a protective impact on the mental health of low-income Canadians. CERB provided Canadians who lost employment during the pandemic with a $2000 monthly income. For some low-income individuals and households, this would actually increase their monthly income, thereby reducing financial-related stress among this population,” said co-author Maria Rowsell, a research assistant at the University of Toronto’s ILCA.
The study was conducted using data from the Canadian Longitudinal Study on Aging (CLSA) surveys. The CLSA is a large national longitudinal study involving older Canadians with diabetes. This study identified 2,730 individuals with diabetes in the CLSA sample. In this group, 1,757 individuals had no pre-pandemic history of depression, and 973 had a pre-pandemic history of depression. The study was published online this month in the journal Archives of Gerontology and Geriatrics Plus.
“The long-term implications of the pandemic extend far beyond physical health,” said senior author Professor Esme Fuller-Thomson of the University of Toronto’s Factor-Inwentash Faculty of Social Work and Director of the ILCA. “It is important to improve access to mental health services for people with diabetes, particularly during periods of increased stress. Interventions that have shown promising results to support the mental health of individuals with comorbid depression and diabetes include cognitive behavioural therapy and psychoeducation. We need to improve access to these important services.”