
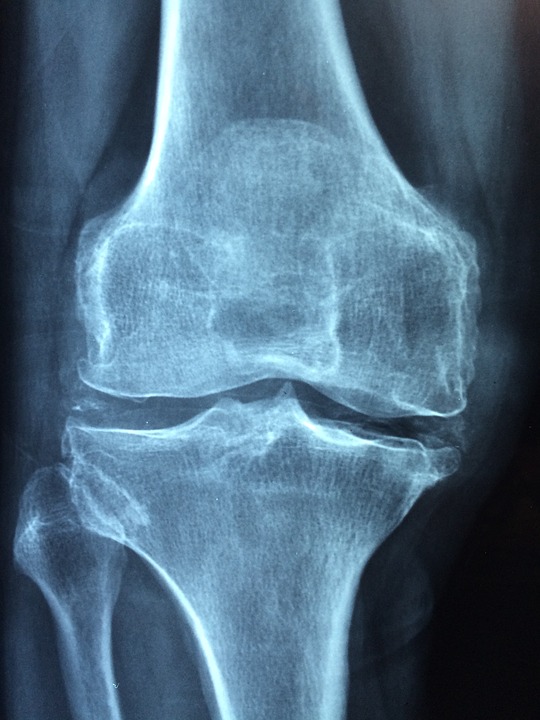
The dynamics of EBV viral capsid antigen (VCA) IgM titers, EBV early antigen-diffuse (EA-D) IgG titers, and serum EBV DNA over time after EBV infection or reactivation. CREDIT Jeffrey E. Gold, Ramazan A. Okyay, Warren E. Licht, and David J. Hurley
Two recently published studies available on the National Institutes of Health (NIH) website indicate Epstein-Barr virus (EBV) reactivation may play a role both in the development of long COVID symptoms, as well as severe COVID-19 cases.
The first evidence linking EBV reactivation to long COVID symptoms was discovered by Gold et al. (2021) and published in Pathogens. This study can be viewed on the NIH website here: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8233978/
“We ran Epstein-Barr virus serological tests on COVID-19 patients at least 90 days after testing positive for SARS-CoV-2 infection, comparing EBV reactivation rates of those with long COVID symptoms to those who never experienced long COVID symptoms,” said lead study author Jeffrey E. Gold of World Organization. “We found over 73% of COVID-19 patients who were experiencing long Covid symptoms were also positive for EBV reactivation.”
Another group of researchers, Chen et al. (2021), found EBV reactivation may also be associated with COVID-19 severity. Their report published in Scientific Reports by Nature is available here: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8149409/
According to Gold, more than 95% of health adults will test positive for latent EBV infection, identified by testing for the presence of EBV VCA IgG and/or EBV nuclear antigen 1 (EBNA-1) IgG. EBV reactivation, on the other hand, is identified by further testing for the presence of EBV EA-D IgG, EBV VCA IgM, and/or circulating EBV DNA.
David J. Hurley, PhD, a professor and molecular microbiologist at the University of Georgia and coauthor of the Pathogens study said, “We found similar rates of EBV reactivation in those who had long COVID symptoms for months, as in those with long COVID symptoms that began just weeks after testing positive for COVID-19. This indicated to us that EBV reactivation likely occurs simultaneously or soon after COVID-19 infection.”
According to Gold, other diseases and stressors can also trigger EBV reactivation, this is not exclusive to COVID-19. The inflammation response from SARS-CoV-2 infection, however, appears more successful than many other stressors at triggering EBV reactivation. While EBV reactivation may not be responsible for all cases of recurring fatigue or brain fog after recovering from COVID-19, evidence indicates that it likely plays a role in many or even most cases.
The Pathogens study found that nearly one-third of 185 people surveyed who had tested positive for COVID-19 ended up with long haul symptoms, even some who were initially asymptomatic. This percentage of long term sequelae after COVID-19 infection was similar to the percentage found in a separate study Sequelae in Adults at 6 Months After COVID-19 Infection published in JAMA Network Open.
The relationship between SARS-CoV-2 and EBV reactivation described in these studies open up new possibilities for the diagnosis and treatment of initial COVID-19 infection as well as long COVID. The researchers of the study in Pathogens indicated that it may be prudent to test patients newly positive for COVID-19 for evidence of EBV reactivation indicated by positive EBV EA-D IgG, EBV VCA IgM, or serum EBV DNA tests. If patients show signs of EBV reactivation, they can be treated early to reduce the intensity and duration of EBV replication, which may help inhibit the development of long COVID.
While there is no available vaccine to prevent EBV infection, on July 26, 2021 a phase 1, open-label study to evaluate the safety and immunogenicity of an EBV vaccine sponsored by the National Institute of Allergy and Infectious Diseases (NIAID) at NIH is expected to begin.
“As evidence mounts supporting a role for EBV reactivation in the clinical manifestation of acute COVID-19, this study further implicates EBV in the development of long COVID,” said Lawrence S. Young, PhD, a virologist at the University of Warwick speaking about the Pathogens study. “If a direct role for EBV reactivation in long COVID is supported by further studies, this would provide opportunities to improve the rational diagnosis of this condition and to consider the therapeutic value of anti-herpesvirus agents such as ganciclovir.”

![Do COVID-19 Vaccines Work for Immunosupprssed People? [Israel Pfizer BNT162b2 Effectiveness Study] - YouTube](https://i.ytimg.com/vi/Ogt1vuiY0g4/mqdefault.jpg)
