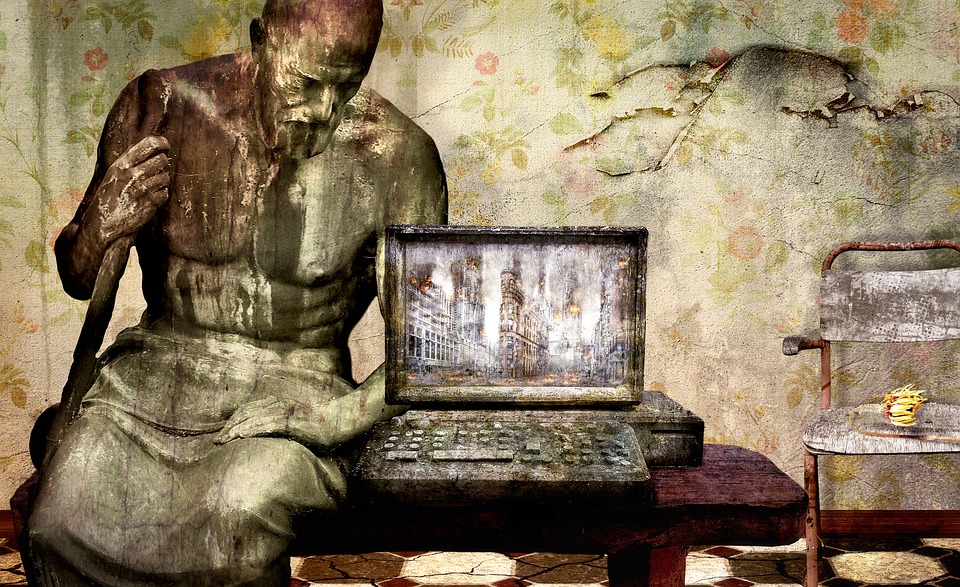
MIT scientists discovered that motor neuron growth significantly increased over five days in response to exercise-related biochemical (left) and mechanical (right) signals. The green ball represents a neuron cluster that extends outward with long tails, known as axons. Credit: Angel Bu.
Exercise is undoubtedly beneficial for the body. Regular physical activity strengthens muscles and enhances bones, blood vessels, and the immune system.
Recent research by MIT engineers has revealed that exercise can also benefit individual neurons. They discovered that when muscles contract during physical activity, they release biochemical signals known as myokines. Neurons exposed to these muscle-generated signals grew up to four times farther than those not exposed to myokines. This cellular-level research indicates that exercise can have a significant biochemical impact on nerve growth.
Researchers made an intriguing discovery: neurons respond not only to the biochemical signals released during exercise but also to the physical stress that occurs during it. They found that when neurons are stretched and then released repeatedly—similar to how muscles contract and expand during physical activity—these neurons grow significantly, just as they do when exposed to myokines produced by the muscles.
Previous studies have suggested a possible biochemical link between muscle activity and nerve growth. However, according to the researchers, this study is the first to demonstrate that physical effects can be equally significant. The findings, set to be published in the journal *Advanced Healthcare Materials*, highlight the relationship between muscles and nerves during exercise. This could lead to the development of exercise-related therapies to repair damaged and deteriorating nerves.
“Now that we understand the existence of muscle-nerve crosstalk, this knowledge could be beneficial for treating conditions such as nerve injuries, where communication between nerves and muscles is disrupted,” explains Ritu Raman, the Eugene Bell Career Development Assistant Professor of Mechanical Engineering at MIT. “By stimulating the muscle, we may be able to encourage the nerve to heal, potentially restoring mobility to individuals who have lost it due to traumatic injuries or neurodegenerative diseases.”
Muscle talk
In 2023, Raman and her colleagues reported that they could restore mobility in mice that had experienced a traumatic muscle injury by implanting muscle tissue at the injury site and then exercising the new tissue by stimulating it repeatedly with light. Over time, they found that the exercised graft helped mice regain their motor function, reaching activity levels comparable to those of healthy mice.
When the researchers analyzed the graft itself, regular exercise appeared to stimulate the grafted muscle to produce specific biochemical signals that promote nerve and blood vessel growth.
“That was interesting because we always think that nerves control muscle, but we don’t think of muscles talking back to nerves,” Raman says. “So, we started to think stimulating muscle was encouraging nerve growth. People replied that maybe that’s the case, but there are hundreds of other cell types in an animal, and it’s hard to prove that the nerve is growing more because of the muscle rather than the immune system or something else playing a role.”
In their new study, the team focused solely on muscle and nerve tissue to determine whether exercising muscles directly affects nerve growth. The researchers grew mouse muscle cells into long fibres that then fused to form a small sheet of mature muscle tissue about the size of a quarter.
The team genetically modified the muscle to contract in response to light. With this modification, the team could flash a light repeatedly, causing the muscle to squeeze in response, mimicking the act of exercise. Raman previously developed a novel gel mat to grow and exercise muscle tissue. The gel’s properties are such that it can support muscle tissue and prevent it from peeling away as the researchers stimulated the muscle to exercise.
The team then collected samples of the surrounding solution in which the muscle tissue was exercised, thinking that the solution should hold myokines, including growth factors, RNA, and a mix of other proteins.
“I would think of myokines as a biochemical soup of things that muscles secrete, some of which could be good for nerves and others that might have nothing to do with nerves,” Raman says. “Muscles are pretty much always secreting myokines, but when you exercise them, they make more.”
“Exercise as medicine”
The team transferred the myokine solution to a separate dish containing motor neurons — nerves found in the spinal cord that control muscles involved in voluntary movement. The researchers grew the neurons from stem cells derived from mice. As with the muscle tissue, the neurons were grown on a similar gel mat. After the neurons were exposed to the myokine mixture, the team observed that they quickly began to grow, four times faster than neurons that did not receive the biochemical solution.
“They grow much farther and faster, and the effect is pretty immediate,” Raman notes.
To examine how neurons changed in response to exercise-induced myokines more closely, the team performed a genetic analysis, extracting RNA from the neurons to determine whether the myokines induced any change in the expression of certain neuronal genes.
“We saw that many of the genes up-regulated in the exercise-stimulated neurons was not only related to neuron growth, but also neuron maturation, how well they talk to muscles and other nerves, and how mature the axons are,” Raman says. “Exercise seems to impact not just neuron growth but also how mature and well-functioning they are.”
The results suggest that exercise’s biochemical effects can promote neuron growth. The group then wondered If exercise’s purely physical impacts could have a similar benefit.
“Neurons are physically attached to muscles, so they are also stretching and moving with the muscle,” Raman says. “We also wanted to see, even in the absence of biochemical cues from muscle, could we stretch the neurons back and forth, mimicking the mechanical forces (of exercise), and could that have an impact on growth as well?”
To answer this, the researchers grew a different set of motor neurons on a gel mat that they embedded with tiny magnets. They then used an external magnet to jiggle the mat — and the neurons — back and forth. In this way, they “exercised” the neurons, for 30 minutes a day. To their surprise, they found that this mechanical exercise stimulated the neurons to grow just as much as the myokine-induced neurons, growing significantly farther than neurons that received no form of exercise.
“That’s a good sign because it tells us both biochemical and physical effects of exercise are equally important,” Raman says.
Now that the group has shown that exercising muscle can promote nerve growth at the cellular level, they plan to study how targeted muscle stimulation can be used to grow and heal damaged nerves and restore mobility for people with neurodegenerative diseases such as ALS.
“This is just our first step toward understanding and controlling exercise as medicine,” Raman says.