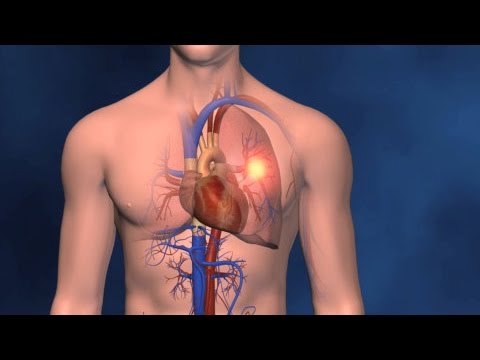
A study conducted at the Center for Research on Redox Processes in Biomedicine (Redoxoma) has enhanced our understanding of how high blood sugar levels (hyperglycemia), a common symptom of diabetes, can lead to thrombosis. The findings, published in the Journal of Thrombosis and Haemostasis, could inform the development of strategies to prevent cardiovascular issues in individuals with diabetes.
“The primary causes of death in Brazil and many other Latin American countries are ischemic events, including heart attacks and strokes, where arterial thrombosis plays a significant role. These cardiovascular disorders can result from various risk factors such as high blood sugar (hyperglycemia), abnormal lipid levels (dyslipidemia), and high blood pressure (hypertension). Among these factors, hyperglycemia is notably associated with an increased risk of cardiovascular disease,” stated Renato Simões Gaspar, the article’s lead author.
The investigation was conducted with support from FAPESP during Gaspar’s postdoctoral research and led by Francisco Laurindo, the last author of the article. Laurindo is a professor at the University of São Paulo’s Medical School (FM-USP) in Brazil and is also a member of Redoxoma, a Research, Innovation, and Dissemination Center (RIDC) established by FAPESP at the Institute of Chemistry (IQ-USP). Gaspar currently teaches at the State University of Campinas (UNICAMP).
The authors state that prolonged hyperglycemia and diabetic ketoacidosis increase the risk of thrombosis. This is due to their effects on endothelial dysfunction, which refers to changes in the inner lining of blood vessels. These changes can lead to the binding of platelets to the endothelial cells, triggering the formation of blood clots.
The study showed that peri/epicellular protein disulfide isomerase A1 (pecPDI) regulates platelet-endothelium interaction in hyperglycemia through adhesion-related proteins and alterations in endothelial membrane biophysics.
“We found that a pathway for this PDI in endothelial cells mediates thrombosis in diabetes when hyperglycemia is present, involving a specific molecular mechanism, which we identified,” Laurindo said.
PDI is an enzyme that resides in the endoplasmic reticulum and has the classic function of catalyzing the insertion of disulfide bridges into nascent proteins so that they merge in the correct shape, i.e. so that the amino acid chain folds to form the three-dimensional structure that makes the molecule functional. It is also found in the extracellular space as pecPDI, a pool secreted or bound to the cell surface, in various cell types including platelets and endothelial cells. Studies have shown that pecPDI regulates thrombosis in several models.
Biochemical and biophysical modifications
To investigate platelet-endothelium interaction in hyperglycemia, the researchers created a model with human umbilical vein endothelial cells cultured in different glucose concentrations to produce normoglycemic and hyperglycemic cells. They assessed PDI’s contribution using whole-cell PDI or pecPDI inhibitors.
The cells were incubated with platelets derived from healthy donors. The platelets adhered almost three times more in hyperglycemic than normoglycemic cells. PDI inhibition reversed this effect, and the researchers concluded that the process is regulated by endothelial pecPDI.
To better understand the result, they investigated biophysical processes such as endothelial cell cytoskeleton remodelling and found that hyperglycemic cells had more well-structured actin filament fibres than normoglycemic cells. They also measured the production of hydrogen peroxide, an oxidizing compound, because reactive oxygen species are mediators of cytoskeleton reorganization and cell adhesion—hyperglycemic cells produced twice as much hydrogen peroxide as normoglycemic cells.
The researchers then investigated whether cytoskeleton reorganization affected cell membrane stiffness since substrate stiffness increases platelet adhesion. Using atomic force microscopy, they demonstrated that hyperglycemic cells were stiffer than normoglycemic cells.
The microscope images also showed the formation of cell elongations with extracellular vesicles that appeared to separate from the elongations. This observation led the researchers to investigate the secretome – the set of proteins secreted by an organism into the extracellular space – to find out whether it included proteins that enhanced platelet adhesion. “The purpose of this experiment was to detect proteins exclusively expressed by or present in hyperglycemic cells and not in controls or cells treated with PDI inhibitors,” Gaspar explained.
They found 947 proteins in the secretome, from which they selected eight with a role in cellular adhesion. They then silenced gene expression for three of these proteins using RNA interference and arrived at two proteins, SLC3A2 and LAMC1, as modulators of platelet adhesion. SLC3A2 is a membrane protein, and LAMC1 is the gamma subunit of laminin 1, a key extracellular matrix component.