Development of autoimmunity at an early age associated with more aggressive form of the disease in genetically susceptible children, a USF Health-led study suggests
The study lead author was Jeffrey Krischer, PhD, director of the University of South Florida Health Informatics Institute and co-chair for the National Institutes of Health-funded TEDDY consortium.
New findings from the international The Environmental Determinants of Diabetes in the Young (TEDDY) study add to a growing body of evidence indicating that type 1 diabetes is not a single disease. The presentation and, perhaps, cause of autoimmune diabetes differs among genetically high-risk children, the research suggests.
In a cohort study published July 22 in Diabetologia, lead author Jeffrey Krischer, PhD, director of the Health Informatics Institute at the USF Health Morsani College of Medicine, and TEDDY colleagues compared the characteristics of type 1 diabetes diagnosed in children before vs. after age 6. The paper’s senior author was Beena Akolkar, PhD, of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK)
“Our results underscore the importance of taking into account the age at development of multiple autoantibodies when evaluating risk factors for progression to a diabetes diagnosis,” said lead author Dr. Krischer, a Distinguished University Health Professor and co-chair for the National Institutes of Health-funded TEDDY consortium. “When the changing picture of autoantibody presentation is considered, it appears type 1 diabetes at an early age is a more aggressive form of the disease.”
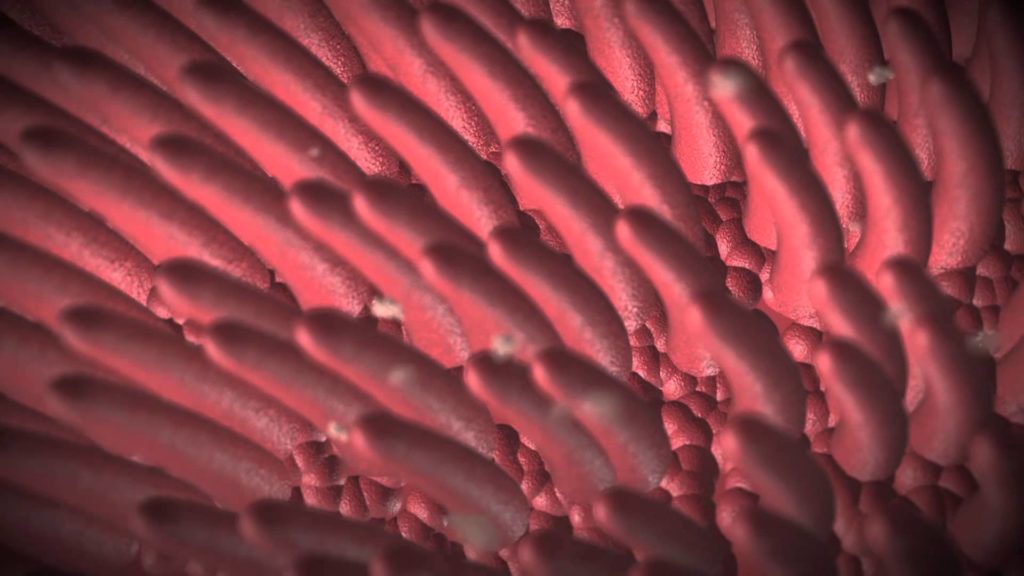
In type 1 diabetes, a misdirected immune response attacks and destroys insulin-producing beta cells in the healthy person’s pancreas – a process occurring over months or many years. Four autoantibodies directed against the pancreatic β-cells — glutamic acid decarboxylase autoantibody (GADA), insulin autoantibody (IA), insulinoma-associated-protein-2 autoantibody (IA2-2A), and zinc transporter 8 autoantibody (ZnT8A) – are thus far the most reliable biological indicators of early type 1 diabetes, before symptoms appear. Not all children who test positive for one or more autoantibodies progress to a diagnosis of type 1 diabetes, which requires lifelong administration of insulin to control blood sugar levels and reduce health complications.
Over the last decade, TEDDY researchers have learned more about how the order, timing and type of autoantibodies can help predict which genetically susceptible children are most likely to get type 1 diabetes as they age.
For this multisite study in the U.S. and Europe, the researchers analyzed data from 8,502 children, all at genetically high risk for developing autoimmunity and type 1 diabetes. The children were followed from birth to a median of 9 years. Over this period, 328 study participants (3.9%) progressed from a presymptomatic stage in which autoantibodies first appeared in their circulating blood (signaling initial autoimmunity) to the onset of symptomatic type 1 diabetes.
Half of the 328 participants (2.0%) were diagnosed before age 6, while the other half (1.9%) developed diabetes between ages 6 and 12. The aim was to determine whether the younger group diagnosed with type 1 diabetes differed from the older group, which would suggest that a different form of type 1 diabetes emerges in children as they grow older.
Among the findings:
- As expected, TEDDY participants who progressed to diabetes between ages 6 and 12 were more likely to have first-appearing autoantibodies to the pancreatic enzyme glutamic acid decarboxylase (GAD autoantibodies), while first-appearing insulin autoantibodies (IA antibodies) were much more common in younger children developing the disease.
- The rate of progression to type 1 diabetes was slower if multiple (two or more) autoantibodies appeared after age 6 than if they were present before age 6.
- The significant association of country of origin with diabetes risk found in the younger group declined in the older group. Conversely, the link between certain genotypes and a higher likelihood of developing diabetes significantly increased in the older children.
- Among children 6 and older with multiple autoantibodies, family history did not appear to play a role in whether the child progressed to type 1 diabetes.
“Much of the observed differences in the relationship between genes and environmental exposures can be explained by the age at appearance of autoantibodies,” Dr. Krischer said. “That is important, because it means factors linked with diabetes risk need to be conditioned on age to be properly understood. There may be different environmental exposures occurring at different ages that trigger autoimmunity, or the same environmental trigger may act differently at different ages.”