Scientists have identified a link between exposure to high levels of oestrogen sex hormones in the womb and the likelihood of developing autism. The findings are published today in the journal Molecular Psychiatry.

The discovery adds further evidence to support the prenatal sex steroid theory of autism first proposed 20 years ago.
In 2015, a team of scientists at the University of Cambridge and the State Serum Institute in Denmark measured the levels of four prenatal steroid hormones, including two known as androgens, in the amniotic fluid in the womb and discovered that they were higher in male foetuses who later developed autism. These androgens are produced in higher quantities in male than in female foetuses on average, so might also explain why autism occurs more often in boys. They are also known to masculinise parts of the brain, and to have effects on the number of connections between brain cells.
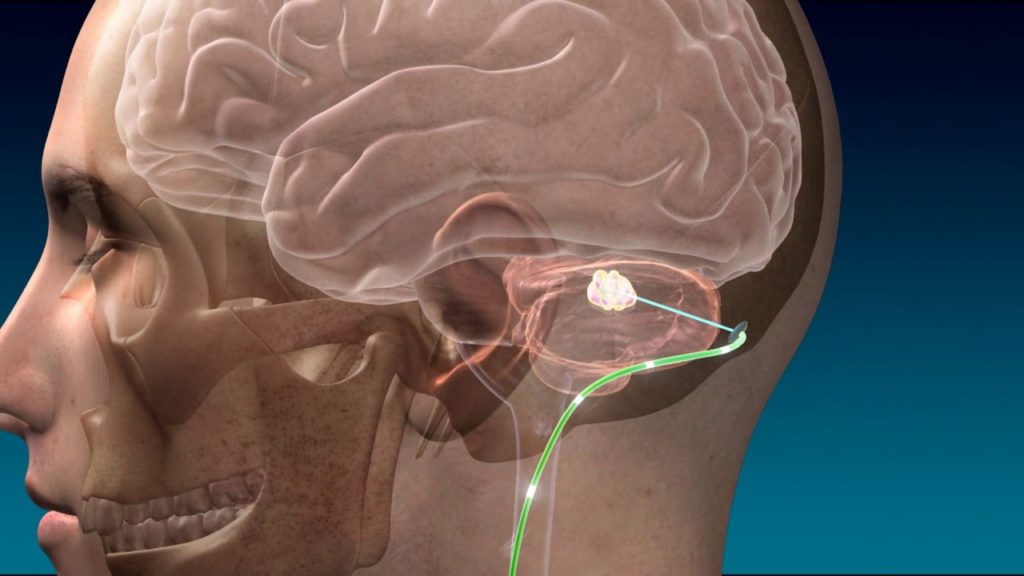
Today, the same scientists have built on their previous findings by testing the amniotic fluid samples from the same 98 individuals sampled from the Danish Biobank, which has collected amniotic samples from over 100,000 pregnancies, but this time looking at another set of prenatal sex steroid hormones called oestrogens. This is an important next step because some of the hormones previously studied are directly converted into oestrogens.
All four oestrogens were significantly elevated, on average, in the 98 foetuses who later developed autism, compared to the 177 foetuses who did not. High levels of prenatal oestrogens were even more predictive of likelihood of autism than were high levels of prenatal androgens (such as testosterone). Contrary to popular belief that associates oestrogens with feminisation, prenatal oestrogens have effects on brain growth and also masculinise the brain in many mammals.
Professor Simon Baron-Cohen, Director of the Autism Research Centre at the University of Cambridge, who led this study and who first proposed the prenatal sex steroid theory of autism, said: “This new finding supports the idea that increased prenatal sex steroid hormones are one of the potential causes for the condition. Genetics is well established as another, and these hormones likely interact with genetic factors to affect the developing foetal brain.”
Alex Tsompanidis, a PhD student in Cambridge who worked on the study, said: “These elevated hormones could be coming from the mother, the baby or the placenta. Our next step should be to study all these possible sources and how they interact during pregnancy.”
Dr Alexa Pohl, part of the Cambridge team, said: “This finding is exciting because the role of oestrogens in autism has hardly been studied, and we hope that we can learn more about how they contribute to foetal brain development in further experiments. We still need to see whether the same result holds true in autistic females.”
However, the team cautioned that these findings cannot and should not be used to screen for autism. “We are interested in understanding autism, not preventing it,” added Professor Baron- Cohen.
Dr Arieh Cohen, the biochemist on the team, based at the State Serum Institute in Copenhagen, said: “This is a terrific example of how a unique biobank set up 40 years ago is still reaping scientific fruit today in unimagined ways, through international collaboration.”
The research was supported by the Autism Research Trust, the Medical Research Council, and Wellcome.