Monash University researchers have uncovered the barrier to β-cell (beta cell) regeneration that could pave the way for improved treatments for diabetes and diseases that involve organ and tissue damage.
The human body doesn’t repair itself very well, with our liver the only organ that can regenerate efficiently. We have limited capacity to regenerate new cells or tissue after birth as the genes involved in development are switched off.
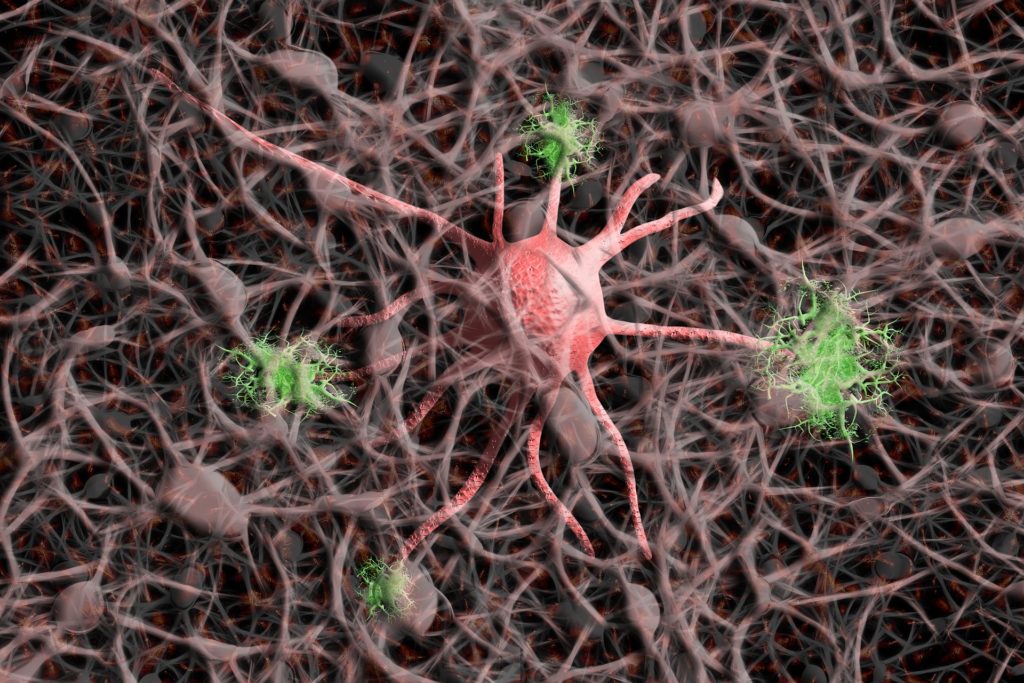
This process happens through DNA methylation, a biological process where chemicals (methyl groups) are written on DNA and modify the way the gene functions. This modification effectively silences genes of progenitor cells (early descendants of stem cells) in the body and thereby the ability for the pancreas to generate the insulin producing β-cells.
Using mouse models, the study published in Regenerative Medicine, led by Professor Sam El-Osta from Monash Central Clinical School, found that the DNA methylation content of two key developmental genes Ngn3 and Sox 11 were diminished, effectively making them ‘repair’ dormant.
However, through demethylation, progenitor cells can be reawakened, restoring their capacity to become new insulin producing beta cells paving the way towards improved treatments for Type 1 and Type 2 diabetes.
“The collaboration between Dr Keith Al-Hasani and Dr Ishant Khurana has unveiled some surprising results. Their discovery that DNA methylation is a barrier to adult beta-cell regeneration will assist scientists to restore beta-cell function in the pancreas,” said Professor El-Osta.
Currently, replacing the damaged β-cell mass in diabetic patients consists of whole pancreas or islets transplantation. Although efficient, these therapies face the shortage of organ donors together with the associated side effects of immunosuppressive drugs.
Current research focuses on the replacement of the lost β-cells in diabetic patients using several approaches and cell sources. However, critical to exploiting the potential of these regenerative approaches, is understanding how tissue and cellular processes are controlled during development.
Co-first author on the study, Dr Keith Al-Hasani added: “This is a novel and significant finding that will allow us to use these “sleeping beauties” (stem cells like cells) to wake up and become insulin cells to cure diabetes.”