Third Grader Grace Moyers shares the early journey she’s had living with Juvenile Rheumatoid...
Rheumatoid arthritis
A significant indicator of whether a patient with rheumatoid arthritis will improve over...
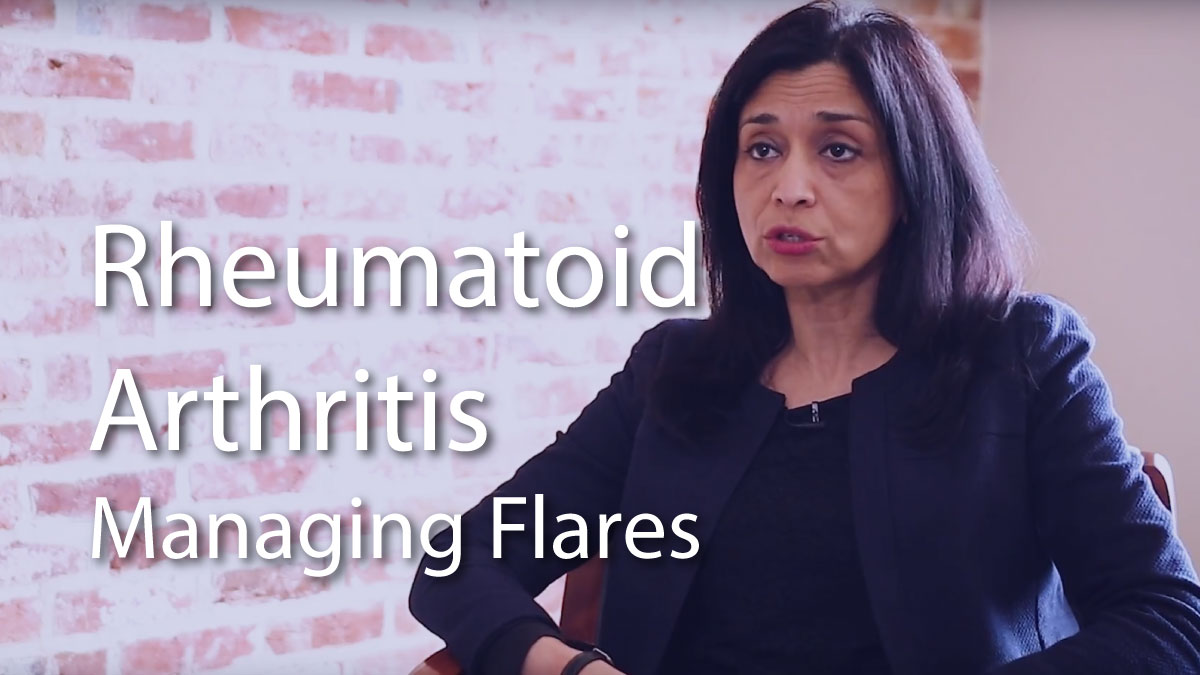
Dr. Uzma Haque goes over some self-management techniques to help alleviate the symptoms of...
reatment options for rheumatoid arthritis have often relied on trial and error. Now Mayo Clinic researchers are exploring...
New research presented at ACR Convergence, the American College of Rheumatology’s annual meeting,...