A newly characterized fat protein could provide the missing link to explain a rare metabolic disease while offering fresh insight into common disorders such as obesity and type 2 diabetes.

Scientists have long sought to find out how some diseases can have symptoms restricted to just one tissue when they are caused by a single faulty protein found throughout the body.
Familial Partial Lipodystrophy type 2 (FPLD2) is a rare disorder causing diabetes, loss of fat in the arms and legs and over development of muscles, yet the faulty protein, lamin A, is found in all cells.
University of Edinburgh scientists found that mice lacking the protein Tmem120a, which is mostly found in fat cells, have similar symptoms as FPLD2.
Tmem120a belongs to a group of proteins, known as NETs, that help ensure the cell’s genetic material, found inside the cell’s command centre – the nucleus – is correctly organised and read.
They found that Tmem120a plays a key role in normal development of fat tissue and healthy metabolism by promoting expression of fat genes and shutting off muscle genes in fat tissue.
These effects appear to be due to Tmem120a’s ability to release parts of the genome that control fat metabolism away from the edge of the nucleus while recruiting muscle genes to the edge.
When genes are at the edge of the nucleus they tend to be shut off and the scientists found that the mispositioning of genes in the mice lacking Tmem120a also occurred in human patients with FPLD2.
The study authors propose that because Tmem120a is found mostly in fat tissue that it mediates the fat-specificity of the defect caused by the faulty lamin A protein previously linked to FPLD2.
Studies on genetic defects that cause metabolic disease indicate they are complex with many genes implicated; thus, Tmem120a, by affecting positioning of many genes, could similarly be involved.
The findings could have wider implications for other metabolic diseases, such as diabetes, insulin resistance, glucose intolerance, and obesity, as well as muscle disorders and body building.
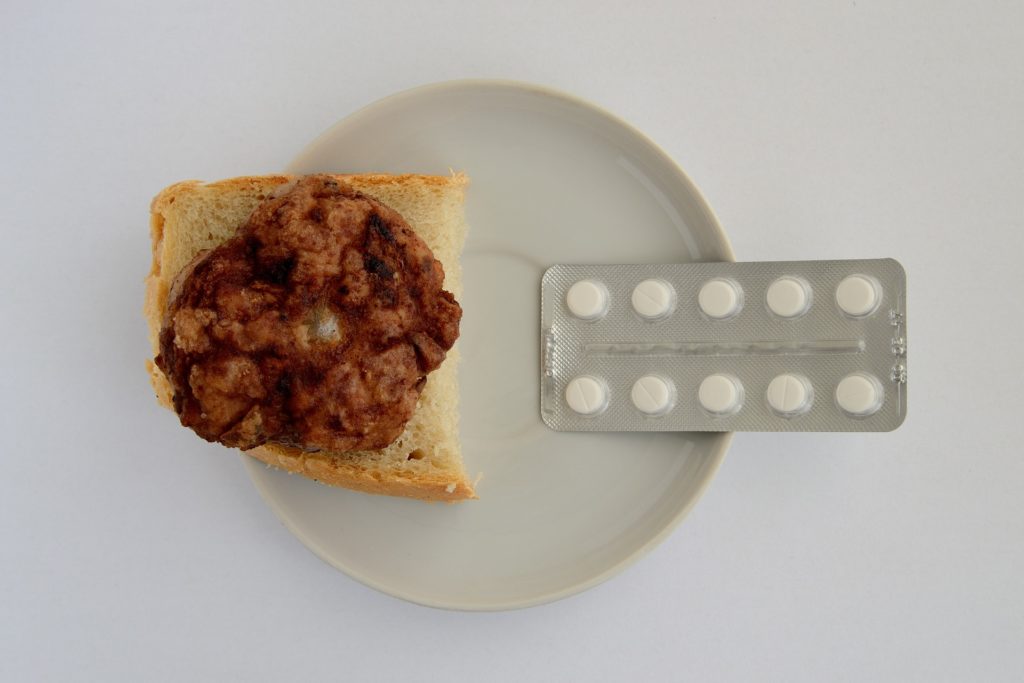
The symptoms only became apparent in mice that were fed a high calorie diet, consistent with the symptoms with FPLD2 which often appear later in life and require a carefully controlled diet.
This mechanism could explain why some diseases such as diabetes are only revealed when the body is under pressure – such as the high calorie diet fed to the mice lacking the Tmem120a gene.
Functional defects in other NET proteins are linked to many human diseases such as muscular dystrophies, cardiomyopathy, blood and bone disorders, cancers, and premature aging syndromes.
Other complex diseases could have a similar mechanism in which NETs affecting gene positioning cause small changes in expression of multiple genes so that pathways still function but at reduced capacity, thus producing symptoms only under certain circumstances.
Dr Rafal Czapiewski, first author and Postdoctoral Research Associate, Institute of Cell Biology, School of Biological Sciences, University of Edinburgh, said:
“The part that is most interesting for me is the discovery of the new mechanism for muscle growth observed in lipodystrophy that opens new potential avenues for increasing muscle mass that is lost for example in astronauts during space travel, in muscular dystrophy or in muscle loss caused by injuries.”