
Fibromyalgia affects millions of people out there and it is not related in any way to a person’s social status. Believe it or not, there are a lot of celebrities out there who live with fibromyalgia as well

Fibromyalgia affects millions of people out there and it is not related in any way to a person’s social status. Believe it or not, there are a lot of celebrities out there who live with fibromyalgia as well

Patients with fibromyalgia syndrome (FMS) typically have widespread chronic pain and fatigue. For those with low vitamin D levels, vitamin D supplements can reduce pain and may be a cost-effective alternative or adjunct to other treatment, say researchers in the current issue of PAIN®.
In addition to pain and fatigue, individuals diagnosed with FMS may experience sleep disorders, morning stiffness, poor concentration, and occasionally mild-to-severe mental symptoms such as anxiety or depression. The condition can have a significant impact on the patient’s quality of life, resulting in loss of employment and/or withdrawal from social life. There is no cure, and no treatment will address all of the symptoms, but some symptoms may be alleviated by physical therapy, cognitive behavioral therapy, temporary drug therapy (such as amitriptyline, duloxetine, or pregabaline) and multimodal therapies.
Calcifediol (also known as calcidiol, 25-hydroxycholecalciferol, or 25-hydroxyvitamin D (OH)D) is a prehormone produced in the liver by the enzyme cholecalciferol (vitamin D3). Calcifediol is then converted to calcitriol (1,25-(OH)2D3), which is the active form of vitamin D. The concentration of calcifediol in blood is considered the best indicator of vitamin D status.
Researchers hypothesized that vitamin D supplementation would reduce the degree of chronic pain experienced by FMS patients with low levels of calcifediol and also might improve other symptoms. “Low blood levels of calcifediol are especially common in patients with severe pain and fibromyalgia. But although the role of calcifediol in the perception of chronic pain is a widely discussed subject, we lack clear evidence of the role of vitamin D supplementation in fibromyalgia patients,” says lead investigator Florian Wepner, MD, of the Department of Orthopaedic Pain Management, Spine Unit, Orthopaedic Hospital, Speising, Vienna, Austria. “We therefore set out to determine whether raising the calcifediol levels in these patients would alleviate pain and cause a general improvement in concomitant disorders.”
In a randomized controlled trial, 30 women with FMS with low serum calcifediol levels (below 32ng/ml) were randomized to a treatment or control group. The goal for the treatment group was to achieve serum calcifediol levels between 32 and 48ng/ml for 20 weeks via oral cholecalciferol supplements. Serum calcifediol levels were reevaluated after five and 13 weeks, and the dose was reviewed based on the results. The calcifediol levels were measured again 25 weeks after the start of the supplementation, at which time treatment was discontinued, and after a further 24 weeks without supplementation.
Twenty-four weeks after supplementation was stopped, a marked reduction in the level of perceived pain occurred in the treatment group. Between the first and the 25th week on supplementation, the treatment group improved significantly on a scale of physical role functioning, while the placebo group remained unchanged. The treatment group also scored significantly better on a Fibromalgia Impact Questionnaire (FIQ) on the question of “morning fatigue.” However, there were no significant alterations in depression or anxiety symptoms.
“We believe that the data presented in the present study are promising. FMS is a very extensive symptom complex that cannot be explained by a vitamin D deficiency alone. However, vitamin D supplementation may be regarded as a relatively safe and economical treatment for FMS patients and an extremely cost-effective alternative or adjunct to expensive pharmacological treatment as well as physical, behavioral, and multimodal therapies,” says Wepner. “Vitamin D levels should be monitored regularly in FMS patients, especially in the winter season, and raised appropriately.”

People who have the common chronic pain condition fibromyalgia often report that they don’t respond to the types of medication that relieve other people’s pain. New research from the University of Michigan Health System helps to explain why that might be: Patients with fibromyalgia were found to have reduced binding ability of a type of receptor in the brain that is the target of opioid painkiller drugs such as morphine.
The study included positron emission tomography (PET) scans of the brains of patients with fibromyalgia, and of an equal number of sex- and age-matched people without the often-debilitating condition. Results showed that the fibromyalgia patients had reduced mu-opioid receptor (MOR) availability within regions of the brain that normally process and dampen pain signals – specifically, the nucleus accumbens, the anterior cingulate and the amygdala.
“The reduced availability of the receptor was associated with greater pain among people with fibromyalgia,” says lead author Richard E. Harris, Ph.D., research investigator in the Division of Rheumatology at the U-M Medical School’s Department of Internal Medicine and a researcher at the U-M Chronic Pain and Fatigue Research Center.
“These findings could explain why opioids are anecdotally thought to be ineffective in people with fibromyalgia,” he notes. The findings appear in The Journal of Neuroscience. “The finding is significant because it has been difficult to determine the causes of pain in patients with fibromyalgia, to the point that acceptance of the condition by medical practitioners has been slow.”
Opioid pain killers work by binding to opioid receptors in the brain and spinal cord. In addition to morphine, they include codeine, propoxyphene-containing medications such as Darvocet, hydrocodone-containing medications such as Vicodin, and oxycodone-containing medications such as Oxycontin.
The researchers theorize based on their findings that, with the lower availability of the MORs in three regions of the brains of people with fibromyalgia, such painkillers may not be able to bind as well to the receptors as they can in the brains of people without the condition.
Put more simply: When the painkillers cannot bind to the receptors, they cannot alleviate the patient’s pain as effectively, Harris says. The reduced availability of the receptors could result from a reduced number of opioid receptors, enhanced release of endogenous opioids (opioids, such as endorphins, that are produced naturally by the body), or both, Harris says.
The research team also found a possible link with depression. The PET scans showed that the fibromyalgia patients with more depressive symptoms had reductions of MOR binding potential in the amygdala, a region of the brain thought to modulate mood and the emotional dimension of pain.
The study subjects were 17 women with fibromyalgia and 17 women without the condition.
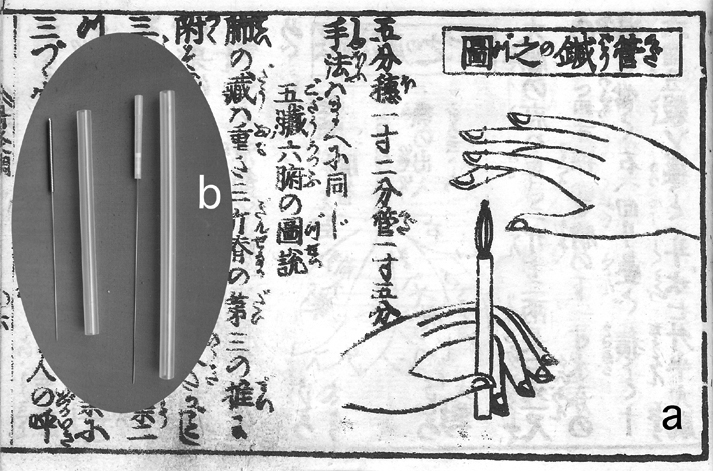
Fibromyalgia patients treated with six sessions of acupuncture experienced significant symptomatic improvement compared to a group given simulated acupuncture sessions according to a new Mayo Clinic study. The findings will be presented at the 11th World Congress of the International Association for the Study of Pain in Sydney, Australia.
“This study shows there is something real about acupuncture and its effects on fibromyalgia,” says David Martin, M.D., Ph.D., Mayo Clinic anesthesiologist and the study’s lead investigator. “Our study was performed on patients with moderate to severe fibromyalgia. It’s my speculation that if acupuncture works for these patients with recalcitrant fibromyalgia — where previous treatments had not provided satisfactory relief — it would likely work for many of the millions of fibromyalgia patients.”
Acupuncture could fill a gap in available therapies for the disease as something additive to what medications already can provide, says Dr. Martin. “There’s not a cure available, so patients are often left somewhat frustrated by continuing pain and fatigue,” he says. “Acupuncture is one of the few things shown to be effective for these symptoms. It may be particularly attractive to patients who are unable to take medications because of intolerable side effects.”
The study, conducted by Mayo Clinic physicians specializing in pain management, included 50 patients diagnosed with fibromyalgia for whom other symptom-relief treatments were ineffective. The patients were randomly assigned to receive acupuncture or simulated acupuncture and were not informed which treatment they received; these treatments were administered in six sessions over two to three weeks.
All patients were given questionnaires before treatment, immediately after treatment, and at one and seven months after treatment to determine the degree of symptoms they experienced and how the disease affected their daily lives.
Patients who received acupuncture experienced minimal side effects. Following treatments, symptoms of pain, fatigue and anxiety were most significantly improved in the patients given acupuncture. At seven months post-treatment, the patients’ symptoms of pain, anxiety and fatigue had returned to baseline levels; the patients experienced the largest improvement at one month following treatment.
“We expected the acupuncture to improve the pain,” says Dr. Martin. “We didn’t really expect the largest benefit to be in fatigue or anxiety.”
Dr. Martin hypothesizes that acupuncture affects symptoms such as anxiety and fatigue because it may target the root cause and not the daily symptoms of fibromyalgia. “In a Western view of medicine, we’re modulating sensory input through acupuncture,” he says. “Whenever there’s an input to the nervous system, it responds and adapts to the input — sometimes in ways that are beneficial to patients. This is not so different from the traditional Eastern explanation of acupuncture that describes needles as altering the flow of life energy, called Qi.”
The Mayo Clinic researchers noted that although the patients saw improvement in symptoms which had reduced activity level, physical function did not increase even though the patients were less tired and felt less pain. “This doesn’t surprise me, as we see this pattern in other chronic pain problems: you can relieve pain, but it’s a lot harder to prompt activity changes,” says Dr. Martin. “A chronically ill person needs more than symptom relief to resume a normal lifestyle. We’re now beginning to work on that problem.”
Dr. Martin indicates that he believes the study patients would have seen sustained improvement with ongoing acupuncture. “It’s a reasonable expectation that if they received more acupuncture after two to three months, they would have maintained their improvement,” he says. “Acupuncture usually works for about three months, and then patients need a less-intensive treatment session. These patients would need more acupuncture periodically for as long as they experience fibromyalgia symptoms.”
The patients were unable to guess whether they had been given the real or the simulated acupuncture. “This was critical, because this had been a shortcoming of other previous studies with acupuncture — the simulated acupuncture treatments were not believable to the patients,” says Dr. Martin.
He explains that fibromyalgia patients have a nervous system disorder in which they have a “revved up pain threshold” which is exacerbated by stress and inadequate sleep. “You can take blood tests, X-rays, muscle tests, and you will find nothing abnormal,” he says. “Many fibromyalgia patients suffer suspicion from their spouses and friends that their symptoms are ‘all in their head’ or that they lack sufficient will or fortitude to meet their obligations to work, family and friends. Usually it comes as a welcome diagnosis when these patients learn it’s fibromyalgia. Then they can learn ways to cope with the disorder and gain strength from sharing with others who have the same problems.”
Dr. Martin describes the patients in this study as moderately debilitated. “Many have given up work, a lot of recreational activities, and made adjustments in their lives,” he says. “They have had a significant psychological burden as a result of the loss of these activities; it’s become part of their identities.”
Dr. Martin says he’d recommend acupuncture for patients who are receptive to the concept. The acupuncture used in this study is available in most communities. Dr. Martin says that to find a qualified acupuncturist, “Talk to your doctor. Many physicians are open to complementary medical techniques and can refer you to qualified practitioners in your area. There are also excellent resources on the Internet from the National Center for Complementary and Alternative Medicine (http://nccam.nih.gov).”
Joining Dr. Martin in this research were Mayo Clinic investigators Christopher Sletten, Ph.D.; Ines Berger, M.D. (currently practicing at the Medical College of Georgia in Augusta); and Brent Williams.
Combining 2 drugs used to treat fibromyalgia safely improves patient outcomes, according to researcher Ian Gilron

Queen’s University researcher Ian Gilron has uncovered a more effective way of treating fibromyalgia, a medical condition characterized by chronic widespread pain typically accompanied by fatigue, as well as sleep, mood and memory problems.
The results of the trial suggest that combining pregabalin, an anti-seizure drug, with duloxetine, an antidepressant, can safely improve outcomes in fibromyalgia, including not only pain relief, but also physical function and overall quality of life. Until now, these drugs have been proven, individually, to treat fibromyalgia pain.
“Previous evidence supports added benefits with some drug combinations in fibromyalgia,” says, Dr. Gilron (Anesthesiology, Biomedical Sciences). “We are very excited to present the first evidence demonstrating superiority of a duloxetine-pregabalin combination over either drug alone.”
Fibromyalgia was initially thought to be a musculoskeletal disorder. Research now suggests it’s a disorder of the central nervous system – the brain and spinal cord. Researchers believe that fibromyalgia amplifies painful sensations by affecting the level and activity of brain chemicals responsible for processing pain signals.
“The condition affects about 1.5 to 5 per cent of Canadians – more than twice as many women as men. It can have a devastating on the lives of patients and their families,” explains Dr. Gilron. “Current treatments for fibromyalgia are either ineffective or intolerable for many patients.”
This study is the latest in a series of clinical trials – funded by the Canadian Institutes of Health Research (CIHR) – that Dr. Gilron and his colleagues have conducted on combination therapies for chronic pain conditions. By identifying and studying promising drug combinations, their research is showing how physicians can make the best use of current treatments available to patients.
“The value of such combination approaches is they typically involve drugs that have been extensively studied and are well known to health-care providers,” says Dr. Gilron.
This new research was published in the journal Pain.
Dr. Gilron and his research team at Queen’s are members of the SPOR Network on Chronic Pain. The national network, funded under Canada’s Strategy for Patient-Oriented Research, directs new research, trains researchers and clinicians, increases access to care for chronic pain sufferers, and speeds up the translation of the most recent research into practice.