Behçet’s disease, or Behçet’s syndrome, is a rare and poorly understood condition that results in inflammation of the blood vessels and tissues.
Confirming a diagnosis of Behçet’s disease can be difficult because the symptoms are so wide-ranging and general (they can be shared with a number of other conditions).Symptoms of Behçet’s disease
The main symptoms of Behçet’s disease include:
genital and mouth ulcers
red, painful eyes and blurred vision
acne-like spots
headaches
painful, stiff and swollen joints
In severe cases, there’s also a risk of serious and potentially life-threatening problems, such as permanent vision loss and strokes.
Most people with the condition experience episodes where their symptoms are severe (flare-ups or relapses), followed by periods where the symptoms disappear (remission).
Over time, some of the symptoms can settle down and become less troublesome, although they may never resolve completely.
Read about the symptoms of Behçet’s disease.
Diagnosing Behçet’s disease
There’s no definitive test that can be used to diagnose Behçet’s disease.
Several tests may be necessary to check for signs of the condition, or to help rule out other causes, including:
blood tests
urine tests
scans, such as X-rays, a computerised tomography (CT) scan or a magnetic resonance imaging (MRI) scan
a skin biopsy
a pathergy test – which involves pricking your skin with a needle to see if a particular red spot appears within the next day or two; people with Behçet’s disease often have particularly sensitive skin
Current guidelines state a diagnosis of Behçet’s disease can usually be confidently made if you’ve experienced at least three episodes of mouth ulcers over the past 12 months and you have at least two of the following symptoms:
genital ulcers
eye inflammation
skin lesions (any unusual growths or abnormalities that develop on the skin)
pathergy (hypersensitive skin)
Other potential causes also need to be ruled out before the diagnosis is made.
Causes of Behçet’s disease
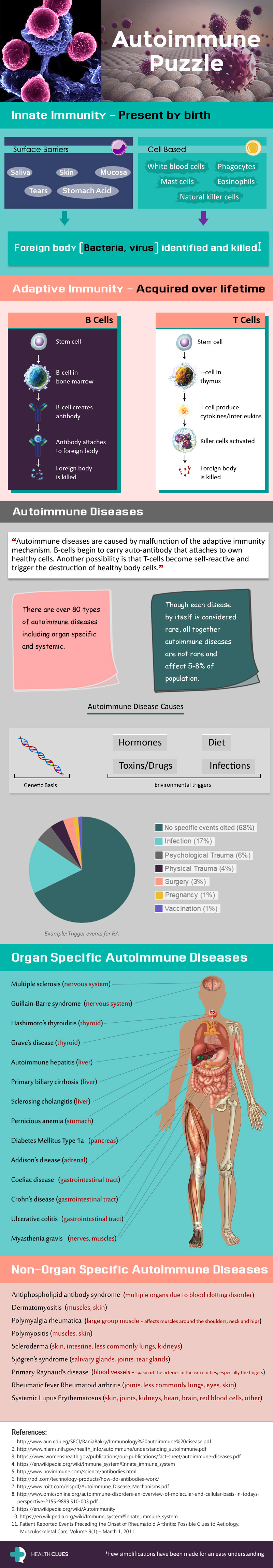
The cause of Behçet’s disease is unknown, although most experts believe it’s an autoinflammatory condition.
An autoinflammatory condition is where the immune system – the body’s natural defence against infection and illness – mistakenly attacks healthy tissue.
In cases of Behçet’s disease, it’s thought the immune system mistakenly attacks the blood vessels.
It’s not clear what triggers this problem with the immune system, but two things are thought to play a role:
genes – Behçet’s disease tends to be much more common in certain ethnic groups where the genes that are linked to the condition may be more common
environmental factors – although a specific environmental factor hasn’t been identified, rates of Behçet’s disease are lower in people from an at-risk ethnic group who live outside their native country
Behçet’s disease is more common in the Far East, the Middle East and Mediterranean countries such as Turkey, Iran and Israel.
People of Mediterranean, Middle Eastern and Asian origin are thought to be most likely to develop the condition, although it can affect all ethnic groups.
Treating Behçet’s disease
There’s no cure for Behçet’s disease, but it’s often possible to control the symptoms with products that reduce inflammation in the affected parts of the body.
These include:
corticosteroids – powerful anti-inflammatory medications
immunosuppressants – medications that reduce the activity of the immune system
biological therapies – medications that target the biological processes involved in the process of inflammation
Your healthcare team will create a specific treatment plan for you depending on your symptoms.
Read about treating Behçet’s disease.