In a new study published today in Cell Reports, researchers from the Donald K. Johnson Eye Institute (DKJEI), part of the Krembil Research Institute at University Health Network, have identified previously unknown connections between genetic factors in Autism ).
This neurodevelopmental disorder is associated with a wide range of physiological and behavioural symptoms, including deficits in communication, cognition and motor function, as well as seizures and hyperactivity.
Autism, which affects one in 50 Canadians between the ages of 1-17, has been linked to hundreds of risk genes that could play a role in disease development.
“We still do not know how different genetic risk factors lead to autism, whether they act independently or through similar molecular pathways to cause the condition. We also don’t know when, or even where, in the brain these genes are expressed and cause the cellular defects that leads to autism. Do defects occur during fetal development, after a child is born, or at some later point in their lifespan?” says Dr. Karun Singh, a Senior Scientist at the DKJEI.
“Our goal for this study was to clarify the roles of specific risk genes in autusm , and whether different genes converge onto common pathways that regulate cell functions, such as energy production and metabolism.”
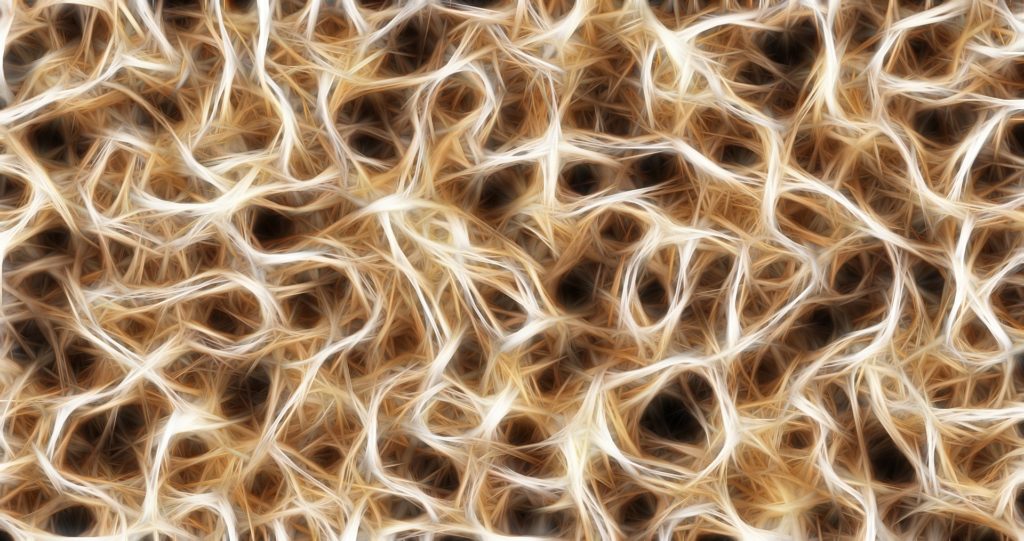
Most autism risk genes produce proteins that are involved in important cellular functions. In this study, the research team used a protein mapping tool to study 41 risk genes associated with autism, many of which were not previously known to interact with each other.
One of the team’s major findings was that several of the risk genes modulate the activity of mitochondria, the energy factories within cells. Since brain cells are metabolically very active, disruptions to their mitochondrial function can impact brain function.
“The link between autism risk genes and mitochondrial dysfunction sheds light on how mutations in these genes might change brain cell activity and ultimately cause disease symptoms,” says Dr. Nadeem Murtaza, a postdoctoral researcher in Dr. Singh’s lab.
The study also revealed that the protein-based mapping tool could be used to help classify individuals with autiusm who have a shared biological signature. Since autism is a highly variable disorder, grouping individuals based on the biological factors underlying their symptoms could help researchers develop more tailored treatments in future.
“There is a lot of opportunity for change to occur between the level of the gene sequences, which we are getting a pretty good handle on, and what actually manifests in the patient,” adds Dr. Murtaza.
“People who have different forms of a genetic disorder might be more connected than we think at the biological level,” says Dr. Murtaza.
The protein-mapping technology used in this study has the potential to improve our understanding of brain function, and can be applied to numerous other brain diseases.
The next step is to apply this technology to patient-specific brain tissue generated in Dr. Singh’s lab, where stem cells from a patient’s blood are developed into three-dimensional brain tissues that exhibit that patient’s unique gene and protein profiles.
“It would enable us to study a patient’s particular disease mechanisms and eventually, test the effectiveness of different therapies,” says Dr. Singh.
“This innovative approach will open the door to these technologies being used more widely and being applied to other diseases as well,” he adds. “Working with colleagues here at Krembil, with programs that span a vast array of neurodegenerative, arthritis and vision-related disorders, is a great way to leverage this technology and our present findings.”