
Did you know there was more than one type of arthritis? Knowing which one you have will get you one step closer to being pain free!

Did you know there was more than one type of arthritis? Knowing which one you have will get you one step closer to being pain free!

In this video, Doctor Andrea Furlan explains that there is a relationship between what we eat and pain. Chronic inflammation may lead to chronic pain, and there are nutrients in our Western diet that predispose to more inflammation. People with autoimmune diseases are prone to more inflammation because their immune system is attacking their own cells using inflammation. We don’t know if fibromyalgia is an autoimmune disease or not, but people with fibromyalgia have more inflammatory markers than people without fibromyalgia.

A new study revealed that a talk therapy practice conducted by telephone could help older adults who have arthritis-related insomnia sleep better. The study was published in the Journal of the American Geriatrics Society.
Why does this matter?
Insomnia is a difficulty in falling or staying asleep. It affects more than 14 million Americans aged 65 and older. It may lead to daytime problems such as tiredness or fatigue, poor concentration, and daytime sleepiness.
Osteoarthritis (OA) is the most common form of arthritis. It can cause or worsen sleep problems. Older adults may develop arthritis after years of wear and tear on their joints, often due to normal physical activity or past injuries. About half of Americans over the age of 65 have been told they have arthritis by their healthcare provider.
What is Cognitive Behavior Therapy?
Cognitive behavioral therapy (CBT) is a type of talk therapy. It can be a fast-acting, long-lasting treatment for insomnia in older adults. In fact, studies suggest that CBT is one of the most effective therapies for insomnia. During CBT sessions, you learn to develop new sleep habits and to identify and change any unhelpful sleep habits.
What the Researchers Learned from this Study
The researchers’ interest in this study was inspired by earlier studies that showed strong evidence that cognitive behavioral therapy is an effective treatment for insomnia. A growing body of evidence suggests that CBT is an especially successful treatment for insomnia that is related to arthritis discomfort.
However, CBT treatment typically requires weekly visits to a therapist’s office, often over several months. For older adults who have insomnia and arthritis, attending therapy sessions in person can be difficult or even impossible.
In this new study, researchers showed that having brief CBT sessions over the telephone was effective for improving arthritis-related insomnia and fatigue over 12 months. They said that the results of their trial showed that telephone CBT reduced the clinical and financial burdens of in-person, arthritis-related CBT insomnia treatment.
Research has shown that telephone CBT can also successfully treat smoking cessation and depression. These results have prompted some health insurance providers to cover CBT phone treatment for certain conditions.
How the Researchers Conducted this Study
The researchers recruited 325 adults aged 60 and over who had moderate to severe insomnia and arthritis pain. The participants were randomly selected to receive one of two treatments. One group received six CBT telephone sessions each week for eight weeks. These participants received coaching on sleep restriction, sleep hygiene, and learned how to restructure their sleep behavior. Participants also got homework assignments to perform.
Participants in the second treatment group received information about sleep and arthritis but did not receive any CBT sleep coaching. Both groups kept sleep diaries.
The researchers collected information on how the participants rated their general health and quality of life according to standard questionnaires. The participants ranked their insomnia status as well as their arthritis pain, stiffness, and ability to function.
After the sessions ended, the researchers said that the people in the CBT group showed improvements in sleeplessness and pain compared to those in the education-only group. They estimated that the cost for the CBT sessions was about $200 per person.
Study Limitations
According to the researchers, no studies exist to show whether CBT for arthritis-related insomnia is a cost-effective treatment. Experts say that there is a strong need for further study in this area. The researchers suggest that further study will help insurers and health care providers decide upon the best treatment decisions and evaluate the cost-effectiveness of CBT telephone treatment for arthritis-related insomnia.
What this Study Means for You
The researchers concluded that phone-delivered CBT significantly improved sleeplessness and pain without increasing total healthcare costs. The researchers said that their findings should encourage healthcare practitioners to consider telephone CBT treatment of insomnia for older adults who also have arthritis.
In a paper published today in the journal Science Translational Medicine, researchers at the Schroeder Arthritis Institute, part of University Health Network (UHN) in Toronto, have made a discovery that could lead to new treatments for axial spondyloarthritis (SpA), a painful and debilitating form of arthritis which affects 1-2% of Canadians and causes inflammation in the spine, joints, eyes, gut and skin.
“We currently have very few therapeutic options for the majority of patients living with SpA and this is a devastating disease that directly impacts quality of life,” says Dr. Nigil Haroon, a rheumatologist, Co-Director of the spondylitis program and senior author on the paper.
“Although several treatments including biologic drugs have been approved for SpA, 40-50 % of patients do not respond to any treatments and develop severe pain and abnormal new bone formation,” says Dr. Akihiro Nakamura, first author on the paper and a spondylitis fellow and PhD candidate in Dr. Haroon’s lab. “So, there is a desperate need to find new treatments that are effective and cover all of the clinical symptoms of SpA.”
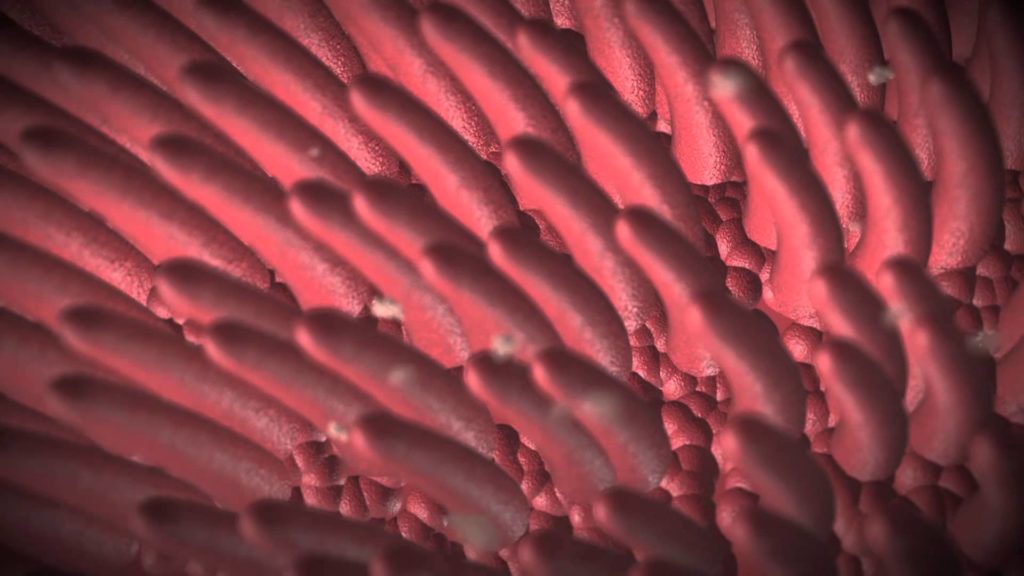
The study focuses on the role of the Macrophage migration inhibitory factor (MIF), which functions as a protein that induces an inflammatory or immune response in the body. Until now, the role that MIF plays in the disease progression of SpA was unknown.
In this study, researchers observed that the expression of MIF and its receptor CD74, is increased in the blood and tissues of pre-clinical models. They also found that human neutrophils (a type of white blood cell that induces the immune system’s response) from SpA patients secreted higher concentrations of MIF, compared to healthy individuals. This, in turn, drives other cells to cause more inflammation.
“What this means is that if the body has been exposed to a trigger, too much MIF could be produced in susceptible individuals that could then lead to a diagnosis of SpA later in life. If we can block the excess production of MIF early, we may be able to induce disease remission and prevent disability and mortality linked to SpA,” explains Dr. Haroon.
In a 2017 paper, the researchers found that the concentration or expression of MIF is substantially increased in the blood, joint fluids and gut tissues of SpA patients, compared to those of a different type of arthritis patients or healthy volunteers. In the same paper, they also demonstrated that MIF might be involved in promoting the development of new bone formation. These recent findings have helped to solidify those results and take our understanding of the role of MIF in SpA, further.
The specific blocker of MIF, called MIF098, successfully prevented and restricted the disease onset and development of SpA, in the pre-clinical model. The team will focus now on testing the potential of other therapies targeting MIF, which could lead to finding a novel treatment in SpA.
“Patients with SpA experience inflammation, pain, stiffness and over time, this can lead to spinal fusion and loss of mobility. But it’s not just the disease itself that these patients have to worry about,” says Dr. Haroon. “Compared to the general population, there is also a 60% increased chance of stroke, and a 30% increase that they may experience a cardiovascular event or a mental illness.”
For Dr. Nakamura, a clinician from Japan who came to the Schroeder Arthritis Institute to become a leading researcher in the area of inflammatory arthritis, these new findings are nothing short of ‘exciting.’
“In research, once we make a new discovery, that has the potential to help many more patients than I could in my clinic, back in Japan,” says Dr. Nakamura. “So that motivates me a lot.”
Researchers are next hoping to test the efficacy of MIF blockers in patients with SpA through clinical trials, where they would look to determine the optimal concentration and administration frequency of MIF-targeted drugs for humans, as well as study potential side effects, to ensure safety.
“The drugs we have currently don’t work for half of all SpA patients,” says Dr. Haroon. “At the same time, rates of arthritis are going up worldwide. We believe this treatment could be effective for a good proportion of SpA patients including those who don’t respond to other currently available treatments.”

In this video, I share a sleep posture arthritis tip my physical therapist taught me years ago to stop shoulder pain in bed. It was a lifesaver for me when sleeping became unbearable due to shoulder pain caused by rheumatoid arthritis and bicep tendonitis.
Have you experienced shoulder pain when sleeping?