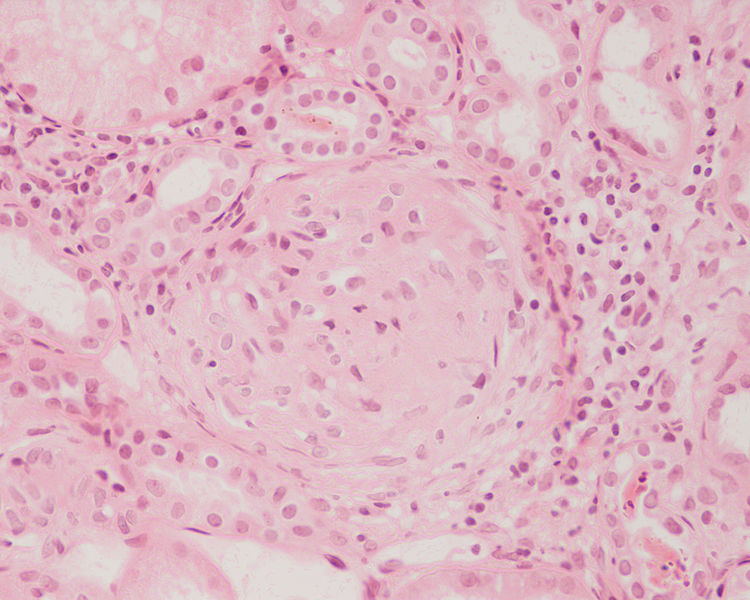
Glomerulonephritis
Glomerulonephritis is damage to the tiny filters inside your kidneys (the glomeruli). It’s often caused by your immune system attacking healthy body tissue.
Glomerulonephritis doesn’t usually cause any noticeable symptoms. It’s more likely to be diagnosed when blood or urine tests are carried out for another reason.
Although mild cases of glomerulonephritis can be treated effectively, for some people the condition can lead to long-term kidney problems.
Symptoms of glomerulonephritis
In severe cases of glomerulonephritis, you may see blood in your urine. However, this is usually noticed when a urine sample is tested.
Your urine may be frothy if it contains a large amount of protein.
If a lot of protein leaks into your urine, swelling of the legs or other parts of the body (oedema) can also develop. This is known as nephrotic syndrome.
Depending on your type of glomerulonephritis, other parts of your body can be affected and cause symptoms such as:
- rashes
- joint pain
- breathing problems
- tiredness
Many people with glomerulonephritis also have high blood pressure.
When to get medical advice
See your GP if you notice blood in your urine. This doesn’t always mean you have glomerulonephritis, but the cause should be investigated.
If your GP suspects glomerulonephritis, they'll usually arrange:
- a blood test - to measure your creatinine level; if your kidneys aren't working normally, the creatinine level in your blood rises and estimated glomerular filtration rate (eGDR) falls
- a urine test - to check for blood or protein in your urine, either by dipping special strips into a sample of your urine or sending the sample to a laboratory for further testing
If glomerulonephritis is confirmed, further blood tests may be needed to help determine the cause.
If your kidney problem needs to be investigated further, it may be recommended that you have:
- an ultrasound scan - this is to check the size of your kidneys, make sure there are no blockages, and look for any other problems
- a biopsy - this is to remove a small sample of kidney tissue, carried out using local anaesthetic to numb the area; an ultrasound machine locates your kidneys and a small needle is used to take a sample
Causes of glomerulonephritis
Glomerulonephritis is often caused by a problem with your immune system. It's not clear exactly why this happens, although sometimes it's part of a condition such as systemic lupus erythematosus (SLE) or vasculitis.
In some cases, the immune system abnormalities are triggered by an infection, such as:
- HIV
- hepatitis B and hepatitis C - viral infections of the liver
- infection of the heart valves (endocarditis)
In most cases, glomerulonephritis doesn't run in families.
If you're diagnosed with an inherited type of glomerulonephritis, your doctor can advise you about the chances of someone else in your family being affected.
They may recommend screening, which can identify people who may be at increased risk of developing the condition.
Treating glomerulonephritis
Treatment for glomerulonephritis depends on the cause and severity of your condition. Mild cases may not need any treatment.
Treatment can be as simple as making changes to your diet, such as eating less salt to reduce the strain on your kidneys.
Medication to lower blood pressure, such as angiotensin-converting enzyme (ACE) inhibitors, is commonly prescribed because they help protect the kidneys.
If the condition is caused by a problem with your immune system, medication called immunosuppressants may be used.
Read about treating glomerulonephritis.
Complications of glomerulonephritis
Although treatment for glomerulonephritis is effective in many cases, further problems can sometimes develop.
These include:
- high blood pressure
- high cholesterol
- blood clots - including deep vein thrombosis (DVT) or a pulmonary embolism
- damage to other organs
- chronic kidney disease
- kidney failure
If you're diagnosed with glomerulonephritis, your doctor may prescribe medication to help lower your blood pressure, lower your cholesterol or protect against blood clots.