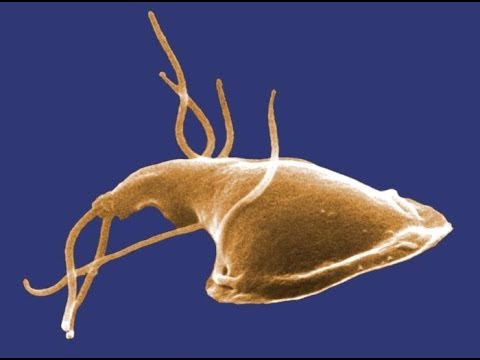
Giardiasis is an infection of the digestive system caused by tiny parasites called Giardia intestinalis (also known as Giardia lamblia, or Giardia duodenalis).
Diarrhoea is the most common symptom of giardiasis.
Other symptoms can include:
abdominal cramps
foul-smelling flatulence and belching
nausea (feeling sick)
bloating
fatigue (extreme tiredness)
loss of appetite
weight loss caused by malnutrition
You may also experience vomiting and a mild fever of 37-38C (98.6-100.4F) but these symptoms are less common.
Although these symptoms are often unpleasant, giardiasis doesn’t usually pose a serious threat to health and can be easily treated.
When to see a doctor
See your GP if you have symptoms of diarrhoea, cramps, bloating and nausea that last for more than a week, particularly if you’ve recently travelled abroad.
If your baby or child has diarrhoea lasting for more than two or three days, or they’ve had six or more episodes of diarrhoea in the last 24 hours, take them to see your GP.
Your GP may have to send stool samples to be tested in a laboratory to diagnose giardiasis. Up to three samples may need to be taken over a number of days to confirm giardiasis.
Treating giardiasis
Giardiasis is usually treated successfully with antibiotic medicine that kills the giardia parasite. In most cases, medicines called metronidazole or tinidazole are used.
Nausea is the most common side effect of metronidazole. On rare occasions, some people may also feel dizzy or sleepy. If this happens to you, avoid driving or using power tools or machinery.
Don’t drink alcohol while taking metronidazole or tinidazole, or for 48 hours after finishing your dose. Mixing alcohol with these types of medication can make the side effects worse.
If you’re diagnosed with giardiasis, other members of your household may be advised to have treatment. This may be recommended as a precautionary measure in case they’ve also been infected. Your GP will be able to tell you if treatment is necessary.
How is giardiasis spread?
Most people become infected with giardiasis by drinking water contaminated with the Giardia parasite, or through direct contact with an infected person.
The giardiasis infection can also be passed on if an infected person doesn’t wash their hands properly after using the toilet, then handles food eaten by others. Food can also be contaminated if it is washed with infected water.
Practising good hygiene – such as regularly washing your hands with soap and water – and taking care when drinking water in countries with poor levels of sanitation can help to reduce your risk of developing giardiasis.
Read more about the causes of giardiasis and preventing giardiasis.
Who is affected?
Giardiasis occurs almost everywhere in the world, but is particularly widespread where access to clean water is limited and sanitation is poor.
It can affect people of all ages but is most common in young children and their parents. This is because things like nappy changing increase the risk of infection.
There are more than 3,500 cases of giardiasis reported in England and Wales each year, although the true number is likely to be higher as many cases go undiagnosed. Around one quarter of these cases are thought to be contracted abroad, but many people don’t develop the symptoms until they return home.
Most cases of giardiasis are one-offs, but small outbreaks can occur in households, among family members, or at nurseries. Larger outbreaks are usually traced to contaminated water sources, such as drinking wells or water parks.
Risk areas for giardiasis
Places where giardiasis is widespread include:
sub-Saharan Africa – all the countries south of the Sahara desert, such as South Africa, Gambia and Kenya
south and southeast Asia, particularly India and Nepal
Central America
South America
Russia
Turkey
Romania
Bulgaria
the countries of the former Yugoslavia (Croatia, Serbia, Montenegro, Slovenia, Macedonia, and Bosnia and Herzegovina)