Otosclerosis is a condition in which there’s abnormal bone growth inside the ear. It’s a fairly common cause of hearing loss in young adults.
There are three tiny bones deep inside the ear, which vibrate when sound waves enter. They transmit sound waves to the cochlea (inner ear), which converts them into signals that are sent to the brain.
In otosclerosis, the stapes (“stirrup” bone) begins to fuse with the surrounding bone, eventually becoming fixed so it can’t move. This means sound is no longer transmitted into the inner ear efficiently.
Symptoms of otosclerosis
Most people with otosclerosis notice hearing problems in their 20s or 30s. One or both ears can be affected.
Symptoms of otosclerosis include:
hearing loss that gets gradually worse over time
particular difficulty hearing low, deep sounds and whispers
speaking quietly because your voice sounds loud to you
finding it easier to hear when there’s background noise (unlike many other types of hearing loss)
tinnitus (hearing sounds such as buzzing or humming that come from inside your body)
dizziness – though this is rare
The symptoms of otosclerosis can be hard to tell apart from other causes of hearing loss.
Is otosclerosis serious?
Otosclerosis can cause mild to severe hearing loss, but it very rarely causes total deafness.
Your hearing usually gets worse gradually over months or a few years and may continue to get worse if ignored and left untreated.
However, the hearing loss can normally be treated successfully with either hearing aids or surgery (read about treatments below). Hearing is improved or restored in around 80-90% of people who have surgery.
Very occasionally, otosclerosis can spread to the inner ear, resulting in a greater level of hearing loss that can’t be improved with surgery.
When to get medical advice
See your GP if you’re worried about your hearing.
They will ask about your symptoms, examine your ears, take your medical history and may do some simple hearing tests.
If your GP suspects a problem such as otosclerosis, you’ll be referred to an ear, nose and throat (ENT) specialist or an audiologist (hearing specialist) at a nearby hospital.
The specialist will carry out some further hearing tests and possibly a scan of your head to help identify the problem.
Treatments for otosclerosis
Otosclerosis can usually be treated successfully with either a hearing aid or surgery. If your hearing loss is very mild, you may not need any treatment at first.
Hearing aids
A hearing aid is an electronic device that increases the volume of sound entering your ear so you can hear things more clearly.
The advantage of using a hearing aid is that, unlike surgery, it doesn’t carry any risks. Modern hearing aids are small and discreet, and some can be worn inside your ear so they’re not obvious.
You can talk to an audiologist about the different types of hearing aid available and which may be best for you.
Surgery
Surgery is an option if you would prefer not to wear a hearing aid. The main operation used is called a stapedotomy or stapedectomy.
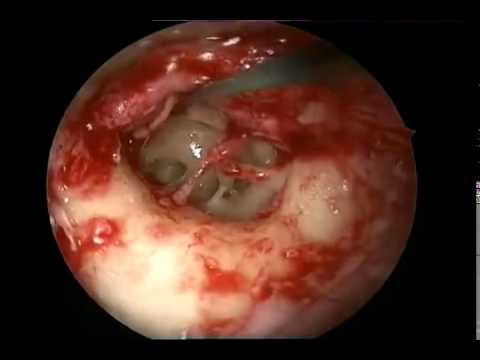
The operation can be done under either general anaesthetic (you’re asleep) or local anaesthetic (you’re awake but your ear is numbed). A cut is made inside your ear canal, or occasionally above or in front of your ear, to access the bones inside your ear.
Part of the stapes bone is removed and a plastic or metal implant is put into the ear to transmit sound from the remaining bones into the inner ear. You’ll be able to go home the same day or the day after.
This is a delicate operation that’s usually very successful. But as with all operations, it carries a small risk of complications, including:
losing more or all of your hearing (in about 1 in 100 cases)
altered sense of taste (usually temporary)
new or worsened tinnitus
vertigo (usually temporary)
facial weakness (very rare)
You can discuss the risks and benefits of both surgery and hearing aids with your surgeon to help you decide which you would prefer.
Causes of otosclerosis
The exact cause of otosclerosis is unclear and it’s not known whether you can do anything to prevent it.
Many cases seem to run in families and it’s thought they may be the result of inheriting a faulty gene from a parent.
The condition can occasionally get worse more quickly during pregnancy, which may mean changes in hormone levels sometimes play a role.