Thyroiditis is swelling (inflammation) of the thyroid gland. It causes either unusually high or low levels of thyroid hormones in the blood.
The thyroid is a butterfly-shaped gland in the neck. It produces hormones that control the body’s growth and metabolism.
These hormones affect processes such as heart rate and body temperature, and convert food into energy to keep the body going.
There are several different types of thyroiditis.
Hashimoto’s thyroiditis
Hashimoto’s thyroiditis is caused by the immune system attacking the thyroid gland, making it swell and become damaged.
As the thyroid is destroyed over time, it becomes unable to produce enough thyroid hormone. This leads to symptoms of an underactive thyroid gland (hypothyroidism), such as tiredness, weight gain and dry skin.
The swollen thyroid may also cause a goitre (lump) to form in your throat.
It may take months or even years for the condition to be detected because it progresses very slowly.
It’s not understood what causes the immune system to attack the thyroid gland. Hashimoto’s thyroiditis is usually seen in women aged 30 to 50 and it sometimes runs in families.
It cannot be cured, but symptoms can be treated with levothyroxine, thyroid hormone replacement medication usually taken for life.
Surgery is needed only rarely – for instance, if your goitre is particularly uncomfortable or cancer is suspected.
Read about treating an underactive thyroid gland and treating goitre.
De Quervain’s (subacute) thyroiditis
De Quervain’s (subacute) thyroiditis is a painful swelling of the thyroid gland thought to be triggered by a viral infection, such as mumps or the flu.
It’s most commonly seen in women aged 20 to 50.
It usually causes fever and pain in the neck, jaw or ear. The thyroid gland can also release too much thyroid hormone into the blood (thyrotoxicosis), leading to symptoms of an overactive thyroid gland (hyperthyroidism), such as anxiety, insomnia and heart palpitations.
These symptoms settle after a few days. Symptoms of an underactive thyroid gland often follow, lasting weeks or months, before the gland recovers completely.
However, if symptoms continue to be severe, the thyroid swelling is one-sided (unilateral), and you continue to have a fever and feel unwell, then you may have infectious thyroiditis.
Palpitations and shakes associated with thyrotoxicosis can be treated with beta-blockers.
To relieve any pain, take over-the-counter painkillers such as aspirin (only if aged 16 or over) or ibuprofen. If these medications do not work, steroids (anti-inflammatory medicine) may be prescribed.
Occasionally, the condition may recur or the low thyroid hormone levels may be permanent, meaning you’ll need long-term thyroid hormone replacement medication.
Postpartum thyroiditis
Postpartum thyroiditis only affects a small number of women who have recently given birth.
However, it is more common in women with type 1 diabetes, positive thyroid antibodies and a previous history of postpartum thyroiditis.
In postpartum thyroiditis, the immune system attacks the thyroid within around six months of giving birth, causing a temporary rise in thyroid hormone levels (thyrotoxicosis) and symptoms of an overactive thyroid gland.
Then, after a few weeks, the gland becomes depleted of thyroid hormone, leading to low thyroid hormone levels and symptoms of an underactive thyroid gland.
However, not every woman with postpartum thyroiditis will go through both these phases.
If low thyroid hormone levels are causing severe symptoms, thyroid hormone replacement medication may be needed until the condition gets better.
If high thyroid hormones are causing symptoms, beta-blockers may provide relief.
In most women, thyroid function returns to normal within 12 months of the birth, although low thyroid hormone levels can sometimes be permanent.
Silent (painless) thyroiditis
Silent thyroiditis is very similar to postpartum thyroiditis, but it can occur in men and women, and is not related to giving birth.
Like postpartum thyroiditis, there may be a phase of high thyroid hormone levels (thyrotoxicosis) causing symptoms of an overactive thyroid gland. This may be followed by symptoms of an underactive thyroid gland, before the symptoms go away in 12 to 18 months.
If low thyroid hormone levels are causing severe symptoms, thyroid hormone replacement treatment may be needed until the condition gets better. In a few cases, the low thyroid levels can be permanent.
Drug-induced thyroiditis
Some medications can damage the thyroid and cause either symptoms of an overactive thyroid gland or symptoms of an underactive thyroid gland. Some examples are interferons (used to treat cancer), amiodarone (for heart-rhythm problems) and lithium (taken for bipolar disorder).
Symptoms are usually short-lived and may get better after you stop taking the medication.
However, you shouldn’t stop taking any prescribed medication without discussing it with your doctor.
Drug-induced thyroiditis can cause pain around the thyroid. This can be relieved with over-the-counter painkillers such as aspirin (only if aged 16 or over) or ibuprofen, although steroids (anti-inflammatory medication) may sometimes be needed.
Radiation-induced thyroiditis
The thyroid gland can sometimes be damaged by radiotherapy treatment or radioactive iodine treatment given for an overactive thyroid gland.
This can either lead to symptoms of an overactive thyroid gland or symptoms of an underactive thyroid gland.
Low thyroid hormone levels are usually permanent, so you may need lifelong thyroid hormone replacement treatment.
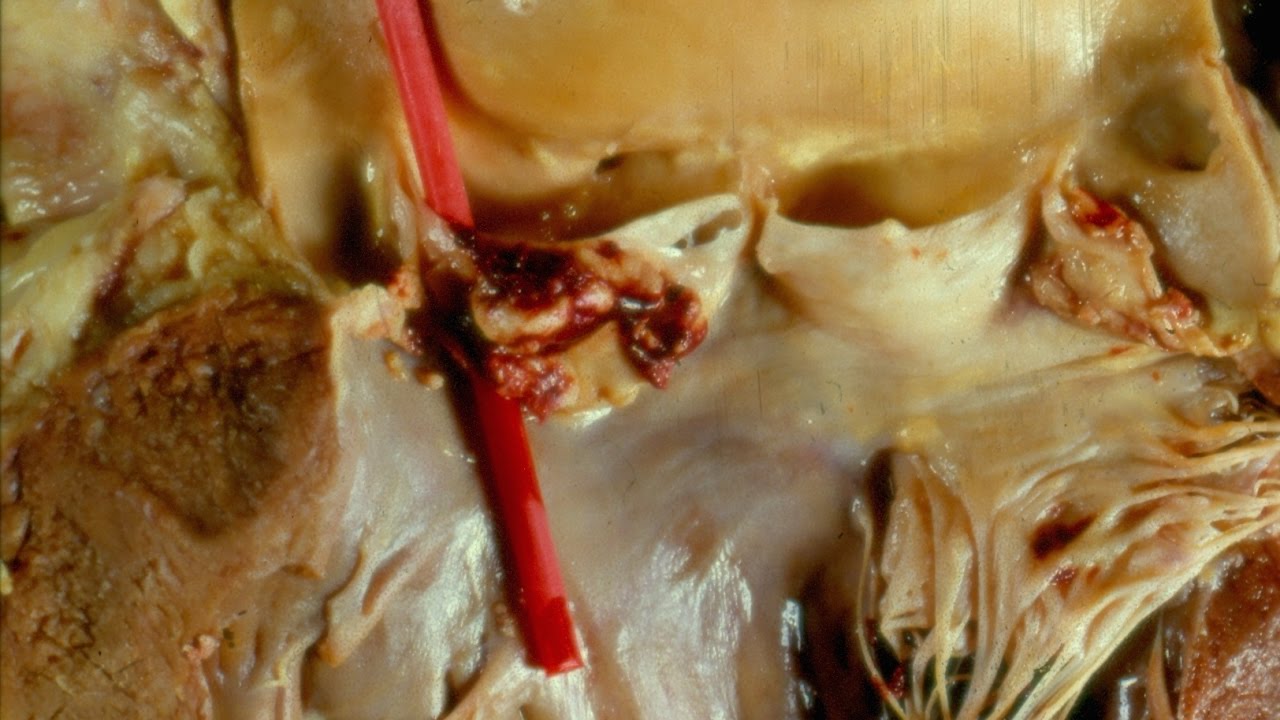
Acute or infectious thyroiditis
Acute or infectious thyroiditis is usually triggered by a bacterial infection. It is rare and is associated with either a weakened immune system or, in children, a problem with the development of the thyroid.
Symptoms may include pain in the throat, feeling generally unwell, swelling of the thyroid gland and, sometimes, symptoms of an overactive thyroid gland or symptoms of an underactive thyroid gland.
Symptoms usually get better when the infection is treated with antibiotics. Thyroid pain can be managed with over-the-counter painkillers such as aspirin (only if aged 16 or over) or ibuprofen.
If symptoms are severe with signs of infection, and particularly if the thyroid swelling appears to be one-sided (unilateral), an ultrasound scan of the thyroid may be needed to check for other problems.
Children usually need an operation to remove the abnormal part of the thyroid.