NB – this was taken from a shared Facebook Post by Vivian Ray Harris
It is so important we felt it was necessary to share. Can we ask that you pass it on as well. It might save a life!
MARKS DEATH:
As most of my friends and family know, my son, Mark, died on May 18, 2017. Due to the manner of his death, we were required to have an autopsy to learn just why he died. We recently received the results of the autopsy. We (his wife, Wendy, and I) want to share the result of that with our family and friends for two reasons.
First, many people thought Mark took his own life. While those of us who spent his last day with him knew this was not the case, without having the autopsy, we really couldn’t say that without knowing why he died. We now know that he died from Serotonin syndrome. On that fateful day he took over the counter cough medicine and it had a fatal interaction with Gabapentin, a drug his doctor prescribed for an off-label use to try to help with his sleepless nights due to the challenges he faced from having Bipolar.
The second reason we wanted to share this is to shed light on Serotonin syndrome. I have worked in the mental health field for over 30 years and have never heard of this syndrome until my son died. Turns out that there are probably many people in this country effected by this syndrome and no telling how many other people have died because of it. If we can make just one person think about their symptoms and seek help before it happens to them or if we can get one doctor to think about the medications they prescribe and how those medications might interact with other medications they are prescribing then some small positive thing can come from our indescribable loss.
Our son died within two hours of symptoms appearing, maybe if we had known what we were seeing and gotten help quicker maybe he would still be with us – we will never know. What we do know is that we loved Mark more than we can ever say – the hole in our hearts will never heal and we don’t want another mother, father, wife, husband, child, brother or sister to lose someone for something that is preventable.
PLEASE SHARE OUR POST WITH ALL YOUR FRIENDS AND ASK THEM TO SHARE IT WITH THEIR FRIENDS. WE WANT THOUSANDS OF PEOPLE TO KNOW ABOUT SERATONIN SYNDROME.
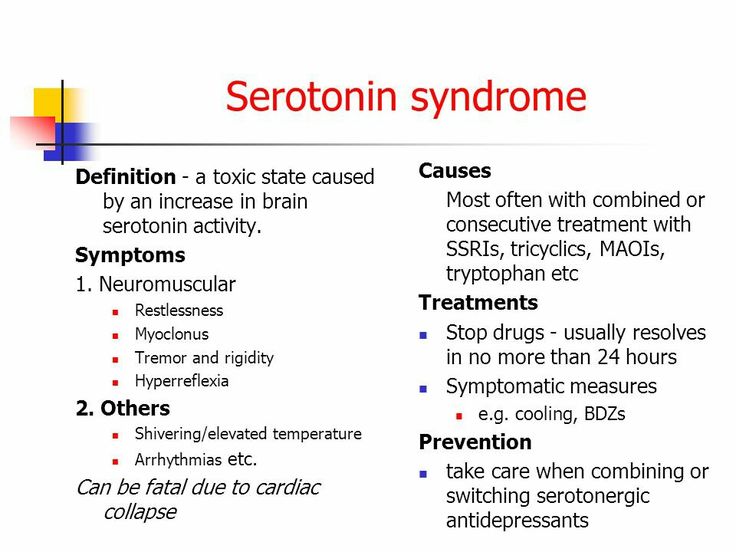
If you take different prescribed medications together, you may end up with too much serotonin in your body. Some of the types of medication that could lead to serotonin syndrome include those used to treat depression, migraine headaches, and manage pain. Too much serotonin can cause a variety of mild to severe symptoms. These symptoms can affect the brain, muscles, and other parts of the body. Serotonin syndrome can occur when you start a new medication that interferes with serotonin. It can also occur if you increase the dosage of a medication you’re already taking. The condition is most likely to occur when two or more drugs are taken together. Serotonin syndrome can be fatal if you don’t receive prompt treatment.
You may have symptoms within minutes or hours of taking a new medication or increasing the dose of an existing medication. The symptoms may include: confusion ,disorientation, irritability ,anxiety, muscle spasms, muscle rigidity, tremors, shivering, diarrhea, rapid heartbeat, or tachycardia, high blood pressure, nausea, hallucinations, overactive reflexes, or hyperreflexia, dilated pupils. In severe cases, the symptoms may include: unresponsiveness, coma, seizures, irregular heartbeat and DEATH.
Please, if you use the types of drugs listed above, please educate yourself – a few websites are below:
https://www.healthline.com/health/serotonin-syndrome…
https://www.mayoclinic.org/…/s…/symptoms-causes/syc-20354758