
There is some confusion about ADHD and Autism, and I’ve received many requests to explain the differences. In this video, I discuss the key differences between the two disorders and how to tell them apart.
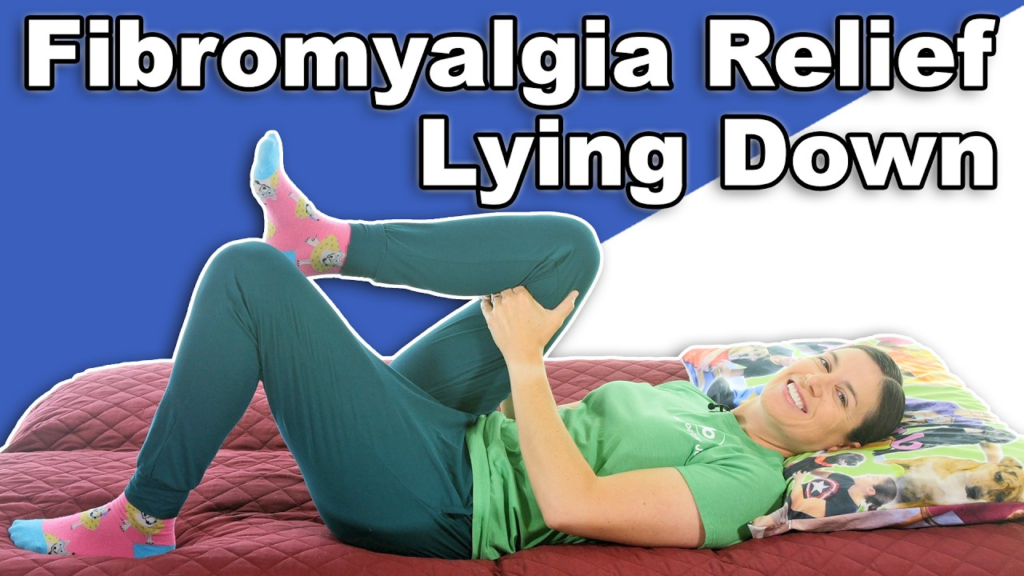
Finding the right intensity of movement to help relieve fibromyalgia and other chronic pain is different from person to person. While movement is important to feeling better, too much can cause a flare-up. The gentle stretches and exercises in this video, when done at one’s own pace, may help relieve the pain. Fibromyalgia and other chronic pain conditions can cause pain, fatigue, sleep disturbances, and even emotional/mental health issues.

Photo by engin akyurt on Unsplash
Neuropathy, the nerve damage that causes pain and numbness in the feet and hands and can eventually lead to falls, infection and even amputation, is very common and underdiagnosed.
“More than one-third of people with neuropathy experience sharp, prickling or shock-like pain, which increases their rates of depression and decreases the quality of life,” said study author Melissa A. Elafros, MD, PhD, of the University of Michigan in Ann Arbor and a member of the American Academy of Neurology. “People with neuropathy also have an increased risk of earlier death, even when you take into account other conditions they have, so identifying and treating people with or at risk for neuropathy is essential.”
The study involved 169 people from an outpatient internal medicine clinic serving mainly Medicaid patients in Flint, Michigan. The participants had an average age of 58 years, and 69% were Black people. One-half of the people had diabetes, which can cause neuropathy. A total of 67% had metabolic syndrome, which is defined as having excess belly fat plus two or more of the following risk factors: high blood pressure, higher than normal triglycerides (a type of fat found in the blood), high blood sugar and low high-density lipoprotein (HDL) cholesterol, or “good” cholesterol. These risk factors are also associated with neuropathy.
All participants were tested for distal symmetric polyneuropathy. Information about other health conditions was also collected.
A total of 73% of the people had neuropathy. Of those, 75% had not been previously diagnosed with the condition. Nearly 60% of those with neuropathy were experiencing pain.
Of those with neuropathy, 74% had metabolic syndrome, compared to 54% of those who did not have neuropathy.
After adjusting for other factors that could affect the risk of neuropathy, researchers found that people with metabolic syndrome were more than four times more likely to have neuropathy than people who did not have the syndrome.
Researchers were also looking for any relationship between race and income and neuropathy, as few studies have been done on those topics. There was no relationship between low income and neuropathy. For race, Black people had a decreased risk of neuropathy. Black people made up 60% of those with neuropathy and 91% of those without neuropathy.
“The amount of people with neuropathy in this study, particularly undiagnosed neuropathy, was extraordinarily high with almost three-fourths of the study population,” Elafros said. “This highlights the urgent need for interventions that improve diagnosis and management of this condition, as well as the need for managing risk factors that can lead to this condition.”
A limitation of the study is that it is a snapshot in time; it did not follow people to see who developed neuropathy over time. It also did not look at why people could not manage risk factors that can lead to neuropathy.
Research led by June Round, PhD, University of Utah, has shown that microbes that live in the gut influence health and social behaviour. CREDIT Charlie Ehlert, University of Utah Health
For autistic people, constipation, diarrhoea, and abdominal pain often go along with the social struggles and repetitive behaviours that define the condition. This has prompted many to wonder whether gastrointestinal (GI) problems arise due to autism’s behavioural or sensory features or whether they might instead contribute to them.
Now, scientists at the University of Utah Health have added to mounting evidence showing that microbes that live in our guts influence behaviour.
The new study, recently published in Nature Communications, demonstrates that it is possible to control-controlled manipulation of the gut microbiome to impact health and behaviour.
“I think that this is a really important step therapeutically because now we can start to assemble a therapy with organisms that we know to be safe,” says June Round, Ph.D., a microbiologist at U of U Health, who led the research.
The Gut-Behavior Connection
Because scientists are still trying to untangle the relationship between GI problems and autism-related behaviours, Round and her team began their study by investigating the behavioural impact of GI distress in mice. Graduate student Garrett Brown, PhD, studied mice with an inflammatory condition called colitis, which causes pain, diarrhoea, and intestinal damage.
After several rounds of colitis, the animals’ symptoms were allowed to subside before behavioural testing. Mice that had experienced colitis moved around normally and showed no signs of anxiety or depression. However, they spent less time interacting with unfamiliar mice than mice that had not experienced colitis. “It’s not like the mice are under so much pain that they’re not doing anything,” Brown says. “So maybe it is something specific to sociability and not just that the mice feel poorly.”
The researchers observed a reluctance to socialize that was reminiscent of the social activities associated with autism. Since their experiments suggested that problems in the gut might drive changes to social behavior, they wondered whether the microbes there—which tend to differ between autistic and neurotypical people—might be involved in both.
To investigate, Brown collected stool samples from people with autism as well as from their neurotypical parents or siblings. Then, he delivered the microbe-filled samples to the GI tracts of mice.
When he induced colitis in those animals, mice carrying microbes from individuals with autism had more intestinal damage and lost more weight than mice whose microbes came from neurotypical individuals. The mix of microbes collected from neurotypical individuals seemed to have a protective effect.
Finding Microbial Protectors
The microbial community inside the human gut is so complex that the team’s samples could easily have included hundreds of kinds of bacteria, viruses, and fungi. Round and Brown wanted to know which community members protected against intestinal problems.
To do that, Brown compared the gut microbes from individuals with autism to those from their neurotypical family members and the microbes living in the guts of mice that had been transplanted with those microbial communities. He was looking for potentially protective microbes that might be underrepresented in people with autism compared to neurotypical individuals—and he found some.
“We were able to pick out individual microbes that we thought might be playing important roles in resisting severe colitis,” explains Brown, who is now a fellow at the National Institutes of Health Clinical Center.
Two in particular stood out. Certain species of Blautia bacteria were better represented in neurotypical individuals than in their autistic family members. And among mice colonized with microbes from autistic people, a group called Bacteroides uniformis was more abundant in those whose colitis was less severe. B. uniformis is known to be underrepresented in people with irritable bowel syndrome and Crohn’s disease, suggesting a role in intestinal health.
Once the researchers had zeroed in on these groups of bacteria, Brown delivered them to mice prior to inducing colitis. Blautia and Bacteroides uniformis reduced intestinal problems, and the Blautia had a corresponding effect on social behaviour. Animals that received the Blautia bacteria were likelier than other mice to engage with unfamiliar mice following colitis.
Toward Personalized Therapies
Round says the study is one of the first to identify specific organisms within the human microbiota that can ameliorate a behavioural deficit associated with GI stress. “This is an example where we are missing microbes, and missing these beneficial microbes is driving disease,” she says.
Further research will be needed to clarify whether boosting the numbers of Blautia or Bacteroides uniformis bacteria might benefit people with GI disorders, autism, or other conditions. But Round says teasing out their individual effects is an important step toward personalized microbiome-targeted therapies.
“One day,” she says, “we’re going be able to quickly analyze the microbiome and say, ‘Hey, you’re missing this really important microbe. We’re going to give it back to you.’”