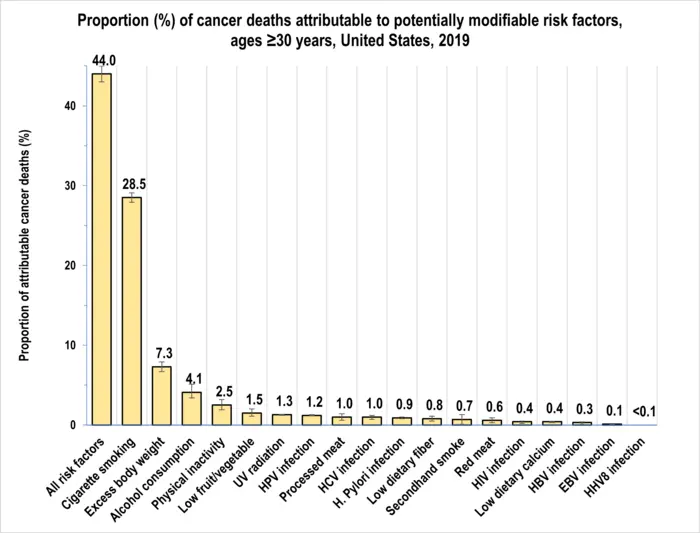
A new study led by researchers at the American Cancer Society (ACS) finds four in 10 cancer cases and about one-half of all cancer deaths in adults 30 years old and older in the United States (or 713,340 cancer cases and 262,120 cancer deaths in 2019) could be attributed to modifiable risk factors, including cigarette smoking, excess body weight, alcohol consumption, physical inactivity, diet, and infections. Cigarette smoking was by far the leading risk factor, contributing to nearly 20% of all cancer cases and 30% of all cancer deaths. The findings are published today in CA: A Cancer Journal for Clinicians.
“Despite considerable declines in smoking prevalence during the past few decades, the number of lung cancer deaths attributable to cigarette smoking in the United States is alarming. This finding underscores the importance of implementing comprehensive tobacco control policies in each state to promote smoking cessation, as well as heightened efforts to increase screening for early detection of lung cancer when treatment could be more effective,” said Dr Farhad Islami, senior scientific director, cancer disparity research at the American Cancer Society and lead author of the report. “Interventions to help maintain healthy body weight and diet can also substantially reduce the number of cancer cases and deaths in the country, especially given the increasing incidence of several cancer types associated with excess body weight, particularly in younger individuals.”
In this study, researchers used nationally representative data on cancer incidence and mortality and risk factor prevalence to estimate the proportion and number of cancer cases and deaths attributable to potentially modifiable risk factors (excluding non-melanoma skin cancers) for 30 cancer types. These risk factors included cigarette smoking (current and former smoking); secondhand smoke; excess body weight; alcohol consumption; consumption of red and processed meat; low consumption of fruits and vegetables, dietary fibre, and dietary calcium; physical inactivity; ultraviolet (UV) radiation; and infection with Epstein-Barr virus (EBV), Helicobacter pylori, hepatitis B virus (HBV), hepatitis C virus (HCV), human herpes virus-8 (HHV-8; also called Kaposi sarcoma herpesvirus), human immunodeficiency virus (HIV), and human papillomavirus (HPV).
The results showed cigarette smoking had the most considerable population-attributable fraction (PAF) or proportion of cancer cases attributable to risk factors in the population (344,070 cases; 19.3% of all cases), contributing to 56.0% of all potentially preventable cancers in men (206,550 of 368,600) and 39.9% in women (137,520 of 344,740). Excess body weight had the second largest PAF (7.6%), followed by alcohol consumption (5.4%), UV radiation exposure (4.6%), and physical inactivity (3.1%).
By cancer type, the proportion of cases caused by potentially modifiable risk factors ranged from 100% for cervical cancer and Kaposi sarcoma to 4.9% for ovarian cancer. It exceeded 50% for 19 of 30 evaluated cancer types. In addition to cervical cancer and Kaposi sarcoma, more than 80% of all melanomas of the skin (92.2%) and cancers of the anus (94.2%), larynx (89.9%), lung and bronchus (lung; 88.2%), pharynx (87.4%), trachea (85.6%), oesophagus (85.4%), and oral cavity (83.7%) were attributable to evaluated risk factors. Lung cancer had the most significant number of cases attributable to evaluated risk factors in both men (104,410 cases) and women (97,250), followed by skin melanoma (50,570), colorectal cancer (44,310), and urinary bladder cancer (32,000) in men and by breast (83,840), corpus uteri (35,790), and colorectal (34,130) cancer in women.
“These findings show a continued need to increase equitable access to preventive health care and awareness about preventive measures. Effective vaccines are available for hepatitis B virus, which causes liver cancer and HPV, which can cause several cancer types, including cervical, other anogenital, and oropharyngeal cancers,” added Dr Ahmedin Jemal, senior vice president of surveillance and health equity science at the American Cancer Society and senior author of the study. “Vaccination at the recommended time can substantially reduce the risk of chronic infection and, consequently, cancers associated with these viruses. HPV vaccination uptake in the United States is suboptimal.”