There may be a way in the future to enhance diabetes treatment – with better control of blood sugar and its use by the brain, and a lower risk for neurological problems – by attaching insulin to a specially designed nanomaterial.
Ohio State University researchers have developed a compound consisting of insulin bound to a string of amino acids that includes an antioxidant group. An earlier study in mice, published in Biomaterials, suggested this nanomaterial’s anti-diabetes properties included improving glucose consumption and availability as fuel for the brain.
In a new study, the team compared the therapeutic effects of the experimental compound to the effects of insulin alone and the nanomaterial alone in mouse models of type 1 diabetes. The measures of blood sugar control and insulin-related gene activity in the brains of mice treated with the combination therapy came close to those of healthy animals, and these same mice did better on tests of their thinking and memory.
Previous research has linked both type 1 and type 2 diabetes to problems with cognitive function and higher risk for dementia, but “neurological complications of diabetes are the least addressed,” said Ouliana Ziouzenkova, associate professor of human sciences at Ohio State and senior author of the study.
“We found in mice that our molecule and insulin combined was better than each treatment alone in reversing diabetes-related problems, and produced a dramatically improved cognitive performance compared to all other groups.”
The research is published in the journal Pharmaceutics.
The molecule the scientists used to bind to insulin’s chemical structure, called AAC2, was developed in the lab of study co-senior author Jon Parquette, professor of chemistry and biochemistry at Ohio State.
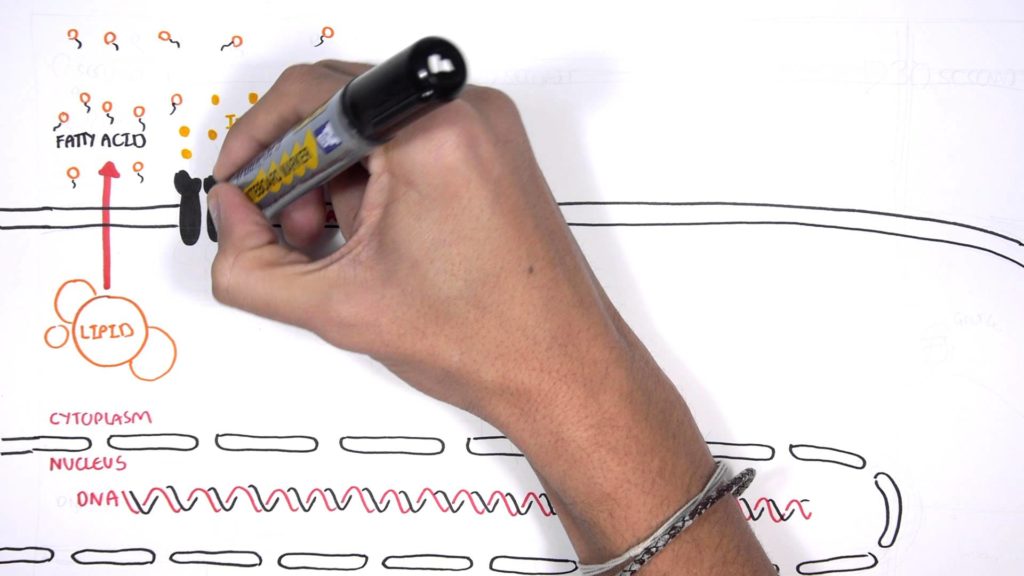
Parquette and collaborators created a series of molecules out of small chains of amino acids and, to make AAC2, the addition of a structural fragment of the antioxidant coumarin. The chains are designed to stack like bricks and stick to each other in a way that enables them to self-assemble into nanofibers that carry a positive electrical charge. The electrical forces hold insulin and AAC2 together to form a supramolecular complex.
“That’s important because of lot of things that happen on a biological scale seem to be on the nanometer scale. Proteins, cell surfaces, viruses are all nanoscale objects,” he said. “So if you can make things that function on that scale you have a better ability to intervene in biological processes.”
The bodies of people with type 1 diabetes don’t make a sufficient amount of insulin, and in people with type 2 diabetes, the body cannot properly use insulin to transfer sugar from the blood to muscle and fat cells, and many other cells in the body, that use glucose for energy. The brain, a major organ requiring the use of glucose for fuel, relies on specific transporters to deliver glucose – transporters whose function can be damaged by irregularities in glucose levels such as those that occur in diabetes.
In this study, experiments were conducted in mice that were chemically and genetically engineered to have insulin deficiencies that cause high levels of blood sugar, the hallmark of type 1 or type 2 diabetes. Researchers injected the animals every three days with either human insulin alone (used to distinguish treatment from insulin produced by the mice), the AAC2 molecule alone, or the AAC2 molecule bound to the human insulin as a combination therapy.
The team found that only the combination therapy produced steady glucose levels in the mice over a long period of time and positively influenced gene expression and neurotransmitter transport in their brains. The mice treated with the combination therapy also performed better on cognitive behavioral tests than animals treated with only insulin or the nanofiber AAC2.
Results suggested that these benefits relate to how insulin’s interactions with the nanomaterial influence two aspects of glucose use in the body: the breakdown of glucose for energy metabolism, and the use of glucose for storage and structural needs. Together, these positive impacts of the therapy can reestablish a healthy energy balance, Ziouzenkova said.
“Our concept provided a balanced metabolic effect involving a completely unique pathway that is induced by this supramolecular complex,” she said.
Research will continue on the exact mechanisms affecting the brain, any long-term side effects and how the compound degrades in the body. Ziouzenkova said the promising findings with diabetes suggest this amino acid-based nanofiber platform may be useful in enhancing treatments for other neurological and metabolic disorders. Kristy Townsend, associate professor of neurosurgery, has joined the research team to explore these directions.