Patients whose Type 2 diabetes is not controlled with metformin can benefit long-term from a two-drug combination treatment that also reduces weight
Patients with Type 2 diabetes often take metformin as first-line therapy to help stabilize their blood glucose. Eventually, some patients no longer respond to metformin and require additional treatment. A few years ago, pivotal short-term trials showed that a combination of two drugs controlled diabetes progression better than either single drug alone. Now, new research demonstrates that this drug combo of dapagliflozin and exenatide continues to stay effective, without loss of effect, after two years of continual use.
“Many therapies in diabetes management are short-lived, which is why it’s useful to test for long-term effect,” says senior author Serge Jabbour, MD, director of the division of endocrinology and the Diabetes Center at Thomas Jefferson University. “Our study showed that a combo regimen of dapagliflozin and exenatide continued to control patients’ glucose for over two years. This is a very encouraging.”
The results of this multi-center double-blind, phase 3, randomized controlled trial were published in the journal Diabetes Care.
A total of 695 adults whose Type 2 diabetes was not controlled with metformin, were randomly assigned to three study groups. One group received weekly exenatide injections in addition to metformin. Another group took daily dapagliflozin pills in addition to metformin, and a third group received both drugs together. The study was an extension study of the pivotal DURATION-8 trial, meaning that patients were given the option to continue in the trial longer.
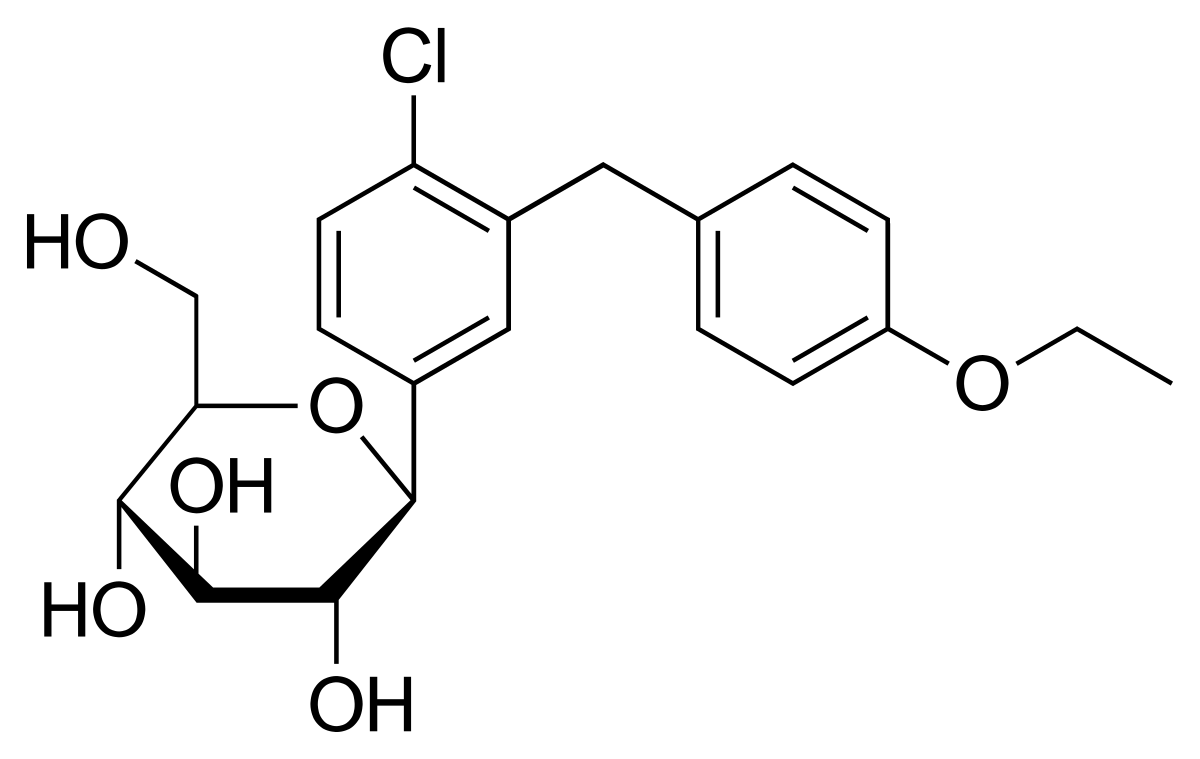
The two classes of drugs act additively, improving the effects on a number of diabetes indicators. Dapagliflozin belongs to a class of drugs called sodium-glucose cotransporter-2 (SGLT2) inhibitors that cause excess glucose to be excreted in the urine. Exenatide belongs to a class of drugs called glucagon-like peptide-1 receptor agonists (GLP-1RAs), which enhance glucose-dependent insulin secretion, lower hepatic glucose output, slow gastric emptying and increase satiety. Together, the two drugs promote and maintain better glucose control and produce additive weight loss and improve blood pressure.
The results confirmed that the group of patients receiving both drugs had better glycemic control than patients receiving just one of the drugs – and demonstrated, for the first time, that the effect was stable for the duration of the extended two-year study period. The study also showed a clinically relevant reduction in weight and blood pressure, measures that can contribute to Type-2 diabetes and overall health. The researchers saw no unexpected safety concerns related to the drug combination in the study participants.
Other studies with both drugs have also suggested that metabolic markers such as lipid profile also improved.
“These two classes work synergistically to help control a Type-2 diabetes patient’s glucose levels, and other measures associated with diabetes,” says Dr. Jabbour. “We can now feel more confident about prescribing these medications long term.”