What if current treatment of insulin resistance was only perpetuating the disease and causing disease to get worse? According to Boston University School of Medicine (BUSM) researchers type 2 diabetes patients are often prescribed drugs that increase insulin release into the blood, which lowers blood glucose but may in fact increase the insulin resistance with long-term use. Many of these patients have elevated insulin even when glucose is normal.
Insulin is the hormone that allows tissues like muscle and fat to take up glucose from the blood to be used as fuel for energy needs. It is released from the pancreas into the blood stream when blood glucose levels increase, such as after a meal. Thus, insulin is secreted to lower blood glucose and keep it at a normal healthy level.
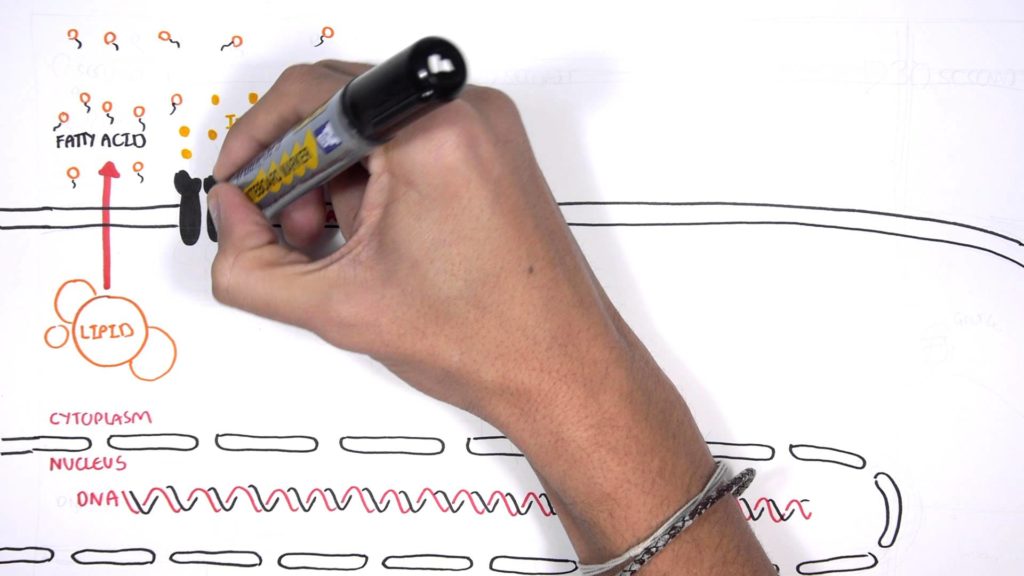
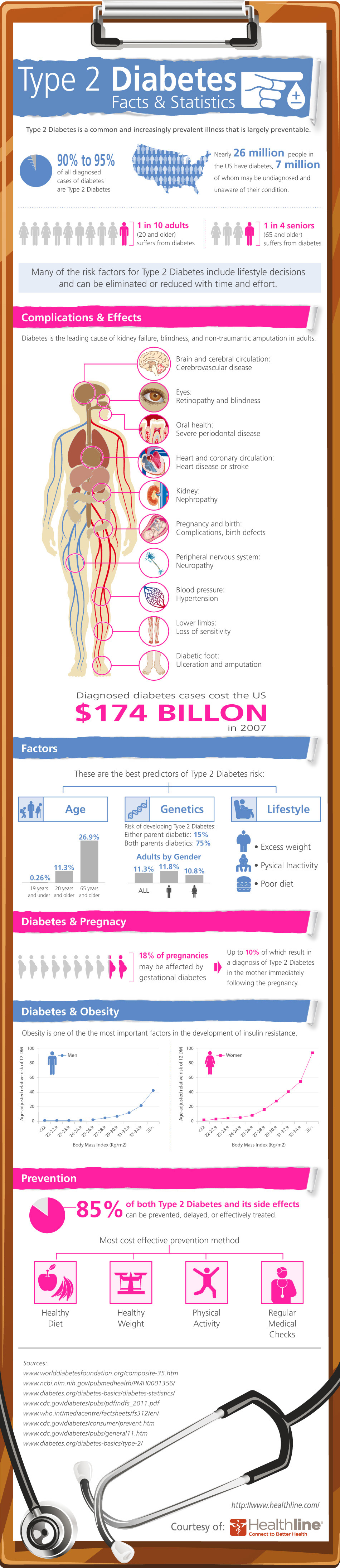
When nutrients such as fatty acid circulate through the blood at a constant high level it can damage tissue function. Insulin resistance is an impairment that occurs in muscle and fat making it harder for insulin to allow these tissues to take up glucose and lower blood glucose to a normal level. As a result, insulin increases to a level that is above normal and remains elevated even between meals and overnight. This causes the pancreas to maintain greater than normal blood insulin levels, a condition known as hyperinsulinemia and that precedes and can result in type 2 diabetes (T2D).
The medical field has long believed that insulin resistance is the root cause of this elevated blood insulin. However, a new review article highlights an opposing view that hyperinsulinemia is initially driven by insulin hypersecretion from beta cells impaired by the excess nutrients and environmental toxins. “Thus increased insulin release from the pancreas drives blood insulin levels higher causing/contributing to insulin resistance,” explains corresponding author Barbara E. Corkey, PhD, professor emeritus of medicine at BUSM.
According to the researchers, T2D patients often are prescribed drugs that increase insulin release into the blood, which lowers blood glucose but may in fact increase the insulin resistance with long-term use. “Our article describes a testable model in which chronic excess nutrient exposure results in insulin hypersecretion from the beta cell contributing to hyperinsulinemia. Hyperinsulinemia normally precedes measurable insulin resistance and T2D. It is viewed by many as a normal response to insulin resistance rather than its potential cause,” says Corkey.
The researchers hope this review will highlight the potential damaging effects of increasing insulin release into the blood when levels are already elevated above normal levels due to insulin resistance. “Rather new therapeutic solutions that include lowering insulin levels before T2D develops may be warranted to prevent insulin resistance further developing into T2D,” said Corkey.