We interviewed to find out more about ulcerative colitis and the treatments avaiable for ulcerative colitis.
PATIENTTALK.ORG -I’m here with Professor Chris Probert, Gastroenterologist of Royal Liverpool Hospital and today we are talking about some new research findings which show that 4 out of 5 people with ulcerative colitis who have had surgery to remove their colon continue to experience symptoms, with around 3 quarter of patients saying the biggest impacts of the disease are on their emotional state. So professor Probert I was wondering if you could please just explain a little bit of about what ulcerative Colitis is and how it differs from Crohn’s disease.
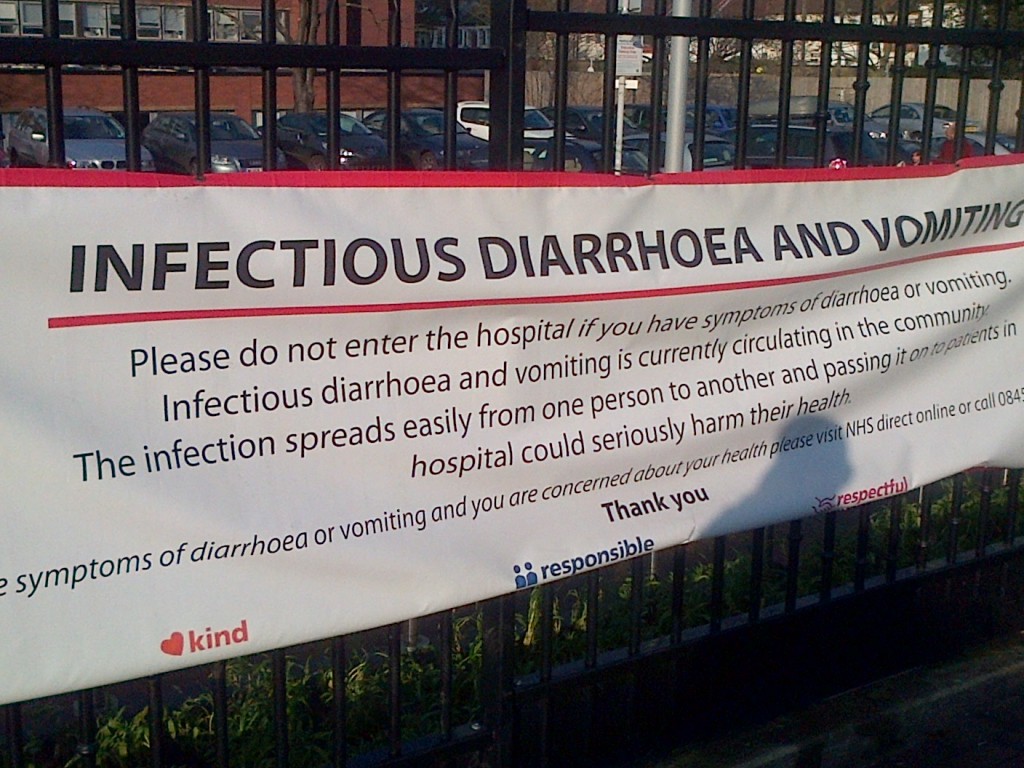
PROF PROBERT – Thank you , ulcerative Colitis is an inflammatory condition affecting the large bowl colon ,and when the colon is inflamed, the patient will experience diarrhoea, cramping and often will bled. Crohn’s disease is a different condition although it’s a bowl inflamed, the small bowl and the large bowl are inflamed in some patients and the disease is quite patchy, so some patients with Crohn’s disease it will just be a small segment of the small bowel, small segment of the large bowl or it can be all over so they are quite different in the distribution and the treatment options are different as well.
PATIENTTALK.ORG -So speaking about distribution, how common is this and how many people are affected by this?
PROF PROBERT – In the UK we think there are about 150 thousand patients with ulcerative Colitis.
PATIENTTALK.ORG -So could you please just run through the early sings of and symptoms that someone would experience if they had ulcerative Colitis undiagnosed?
PROF PROBERT – Patients with ulcerative Colitis will experience initially typically diarrhoea and they will realise this has not gone away the same way as it would with a bug and after a week or two they are starting to start feeling unwell and maybe notice some bleeding, Some patients it can settle down a little bit and then return later, for others it just escalates and it can go from perfect health to life threatening Colitis within a matter of weeks. So there’s a spectrum of ways in which patients present from mild through to moderate.
PATIENTTALK.ORG -Its mentioned in the research that some patients are experiencing a flare up, how often does this lead to hospitalisation?
PROF PROBERT – Patients who have a flare up are the ones who have diarrhoea and bleeding and between the flares hopefully patients are feeling relatively well without too many symptoms. During a flare up if the patient is going to the toilet more then 6 -8 times a day then they should definitely be considered by a specialist to go into hospital, if the patient is feverish then they will clearly need to be in hospital having intravenous therapy as that is a very serious situation potential life threatening situation . Overall about 1 in 10 patients will have a severe flare up at any time.
PATIENTTALK.ORG -So if you’re diagnosed with ulcerative Colitis what sort of life style changes are to be expected and what sort of impact does this have on the people you work with?
PROF PROBERT – Ulcerative Colitis can have a very big impact om patients life’s, if they are lucky enough to have a mild disease it’s a matter of taking the right medication, being a little bit wary , not exposing yourself to the risk of food poisoning and so forth. Patients with a more moderate disease this is starting to get a bit more serious, the treatment will be taken more frequently, they are likely to have steroids more often, they have steroids side effects and that can make you very moody, gain weight and make you feel quite groggy. And for those patients they start to feel rather edgy and insecure you know they don’t know whether the next time they are going to have diarrhoea, they are constantly on the lookout for lavatories and with a country with poor public loos that is a problem, patients know every lavatory between home and school or home and their work place, it makes you very very insecure, it knocks your confidence and constant fatigue.
PATIENTTALK.ORG -Ok so just running through the findings a little bit, the research was done by merk showman limited and what they found was only a third of patients are completely satisfied with their current treatment. So this obviously has something to do with the findings that 4 out of 5 people who have the surgery to have their colon removed are still experiencing the symptoms, so what sort of other options are there? It says here that Nice the medical recommendation of the NHS the body is looking at issuing some guidance on medical options of treatment, would you like to talk about that for a minute?
PROF PROBERT – So patients dissatisfied with therapy we are aware that certain treatments don’t work for everybody and some, despite our best efforts, with conventional therapy will have ongoing symptoms and require repeated courses of surgery, those patients who aren’t settling we need to think about another strategy. For many patients there is a second line group of treatments or surgery, now our concern is that there is a group off treatments that aren’t considered often enough and which at the moment NICE is reviewing, these are the biologic treatments, for patients with disease that’s not settling on conventional therapy a sub group of those will clearly respond to a the biological therapies it will turn the disease off, will prevent surgery in that group of patients, it’s not for everyone but for some patients the biologics will be life transforming. NICE at the moment are saying that this is not a treatment that they are going to support, it’s up for consultation and the consultation closes next Wednesday and we will be very interest if the patients or their relatives who has got an interest in Colitis take the opportunity of going to the NICE website or going to the Crohn’s and Colitis website and making their comments on whether they think this is a good decision. So if NICE say ‘No’ there will be more patients having surgery, if NICE say ‘yes we can use these treatments’ then that small group of patient who needs the treatments we can save an operation.
PATIENTTALK.ORG Can you compare the situation in the UK for treatment purpose with Europe or America? Is there more common use of a medical option in Europe or is the situation broadly similar?
PROF PROBERT – Europe is big place and there is some variation country to country and it depends a lot on what we would call reinvestments and who’s going to pay for the biologic treatments and if the funder is able to support the drug, patients having them results you have heard. North America, the threshold for giving these treatments is substantially lower than in Europe and access to biologic seems a lot easier.
PATIENTTALK.ORG -So it’s in common use in USA?
PROF PROBERT – It is yes
PATIENTTALK.ORG -So is this something that NICE takes into account? Do they look at it being played out in other countries?
PROF PROBERT – No sadly they don’t, NICE have got a very strict way of looking at the world they see how many patients you can treat to get one patient healthy , how much would it cost to teat that community of patients to get that one person healthy, so the cost for an individual may not sound too much but because you have to treat a few more patients who don’t respond, the package of care seems to be rather expensive and so by their estimates it seems to be the package of care costs more than 30 thousand pounds they are going to turn that treatment down and because there are some non-responders to the treatments the cost therefore appears to be higher than that and they are saying no at the moment to everyone , what we would like to purpose is that select out the patients who need it , who are responding to it and you only know perhaps when giving them the treatment for a few weeks couple of cycles), carry on treating those patients who are responding, don’t treat the ones who aren’t responding and that would change the hole dynamic and will change the cost of these treatments to something that might seem acceptable to NICE but at the moment it comes down to economics.
PATIENTTALK.ORG -So anyone who’s interested in this final guidance, you did mention when this would be issued, what was the date for that?
PROF PROBERT – The way to get information on this is to go to the Cohn’s and Colitis website, they have a link to the NICE guidance and you can have a read the full documentation and anyone can upload their comments on the NICE website and consultation closes at 5pm next Wednesday, so anybody listening with Colitis or have got relatives with Colitis who thinks this is important to them should be going to the NICE website, read the documents, make your own mind up and then post your comments.