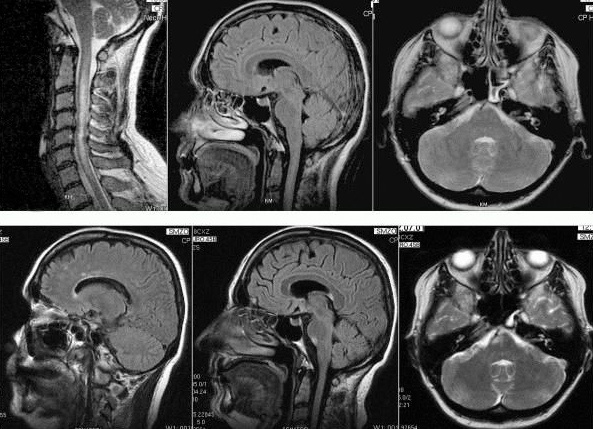
(1) Astrocyte lysis: extensive loss of astrocytes with fragmented and/or dust-like particles; (2) progenitor recruitment: loss of astrocytes except small nucleated cells with GFAP-positive fibre-forming foot processes; (3) protoplasmic gliosis: presence of star-shaped astrocytes with abundant GFAP-reactive cytoplasm; and (4) fibrous gliosis: lesions composed of densely packed mature astrocytes. CREDIT Tohoku University
Researchers in the Department of Neurology at Tohoku University, which is led by professor Masashi Aoki, have developed a classification scheme for neuromyelitis optica spectrum disorder, a rare autoimmune disease that until recently was thought to be a type of multiple sclerosis (MS). The new taxonomy for the disease replaces one borrowed from MS but which was inappropriate for what is in fact a distinct condition.
An autoimmune disease, neuromyelitis optica spectrum disorder (NMOSD), was for a long time thought to be a type of multiple sclerosis (MS), but it has recently been identified as an entirely different illness. As a result of this confusion, identification of NMOSD suffered from a clinical classification scheme borrowed from MS but is inappropriate due to its unique characteristics. A new classification scheme that focuses instead on the degree of deterioration of astrocytes, a specialized central nervous system cell involved in repair processes, has now been developed.
A paper by Yoshiki Takai and Tatsuro Misu at Department of Neurology, Tohoku University, describing the new classification scheme appears online in the journal Brain on March 12.
NMOSD is a rare but serious illness also known as Devic’s disease that produces an inflammation of the spinal cord (myelitis) and optic nerve (optic neuritis) that can lead to blindness and paralysis. Similar to multiple sclerosis, the disorder produces a deterioration of myelin, the fatty layer around neurons that insulates them and allows their electrical impulses to be rapidly transmitted. Deterioration of the myelin slows down or even inhibits this transmission of nerve signals.
As a result of this similarity, NMOSD was long thought to be a sub-type of multiple sclerosis. But NMOSD has recently been identified as a distinct autoimmune illness with more severe symptoms than MS and with a separate set of causes. The demyelinating process in NMOSD is only a product of a newly identified and more fundamental disease process: astrocytopathy, or destruction of astrocytes. These specialized and star-shaped central nervous system cells perform a range of functions, including delivery of nutrients to nervous tissue, regulation of blood flow in the brain, and repair processes after injury or infection.
However, the two diseases, MS and NMOSD, remain difficult for clinicians to distinguish especially in the early stages because both illnesses produce optic neuritis and myelitis.
As a result of this confusion between the two illnesses, up to now, diagnosis of NMOSD has used the same disease classification system as MS, which depends upon the degree of demyelination.
“There was no disease classification system unique and appropriate to this distinct disease,” said Yoshiki Takai of the Department of Neurology at Tohoku University. “So we decided to come up with one ourselves.”
The researchers developed an NMOSD classification scheme that depends not on the degree of demyelination but instead upon differences in the morphology (in essence the shape) of astrocyte degeneration.
This astrocyte degeneration comes in four main types that the researchers have named astrocyte lysis, progenitor, protoplasmic gliosis, and fibrous astrogliosis, each with their own set of characteristic markers identifiable from astrocyte lesions, or damage to the astrocytes. Astrocyte lysis, or extensive loss or complete destruction of astrocytes, a characteristic of the most acute type of such damage (meaning sudden onset and short duration), is a feature highly specific to NMOSD. The other three types describe subacute or chronic forms of the disease (meaning slow onset that can worsen over time).
The classification scheme is the first taxonomy of astrocytopathy to be published.
The researchers hope that in both clinical practice and experimental study, this classification scheme will be used as the standard for all astrocyte-related disease mechanisms both for NMOSD and across the fields of neurodegenerative diseases and neuron regeneration.