Longer working hours coupled with poor hybrid working posture have led to an explosion in back problems amongst younger working adults
The ‘Covid stone’ – the average weight gain during pandemic has been an issue for many Brits, but hybrid working is now taking a toll on our backs. A new national survey[1] and report commissioned by www.mindyourbackuk.com – backed by Mentholatum[2] — makers of a range of evidence-backed topical muscle and joint products and the brains behind a public health initiative – reveals that 64 per cent of 18–29-year-olds have back problems.
With back pain already costing the UK £10 billion per year and accounting for four in ten sick days,[3] it’s clear we need to take action to stop back issues spiralling out of control.
GP and advisor to www.mindyourbackuk.com, Dr Gill Jenkins, says: “For the six in ten Brits who have been mostly or always working from home during the pandemic and are now hybrid working, almost half don’t have constant access to a table and supportive chair during their working day. And unfortunately, 20 per cent have to work while sitting on a sofa or bed. This plays absolute havoc with posture and spine health”.
The www.mindyourbackuk.com survey also found that some workers working from home or hybrid working have been forced to buy their own specialist chairs (17%) as only 11% received work station equipment from their employers.
While the average working day has increased by 48 minutes worldwide[4], many Brits are doing less exercise to compensate for this. A fifth of those polled admitted to doing no exercise at all in a typical working week and just 7 per cent got up to walk around and stretch every hour – which is recommended for desk work.
The reasons for this include a lack of motivation – cited by 46 per cent – and being pushed for time (37 per cent) or lacking energy (26 per cent) – all very bad news for our backs.
Of the people who had experienced new back pain, more than half (56 per cent) said they have lower back pain compared with 23 per cent who have pain in the neck or shoulder blades. Lower back and neck pain are common complaints when screens are not at eye level, or chairs fail to support the back, allowing desk workers to slump.
Dr Jenkins comments: “Caring for our backs can reduce stress and boost energy so we can live our lives to the full, without pains and aches holding us back. We can’t hurry the lockdown easing but we can do things at home to care for our backs. The Mind Your Back 5 S.T.E.P.S. programme[5] keeps your back mobile, flexible and active, and is easy to incorporate into daily life”.
Mind Your Back 5 S.T.E.P.S. programme
Five simple S.T.E.P.S. for home working back care:
- STRETCH – Gentle stretching, even for a few minutes a day, increases mobility and helps loosen tight muscles. Check out 5 stretches at https://www.mindyourbackuk.com/stretch
- THERAPY – hot, cold (or preferably both, alternated) or anti-inflammatory topical therapies (rubs, sprays, patches), such as Deep Heat, Deep Freeze and Deep Relief which help kick-start the healing process.
- EXERCISE – walking, cycling and swimming are all gentle, low impact, exercises that help to mobilise your muscles and joints.
- POSTURE – check your posture, especially while doing desk work or watching TV, to ease non-specific lower back pain and enhance healing
- STRENGTHEN – core and back exercises strengthen back muscles and prevent localised stiffness and pain. See 5 examples at https://www.mindyourbackuk.com/strengthen
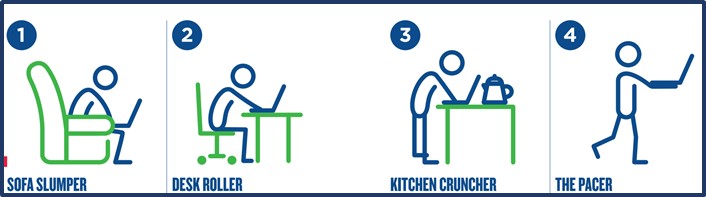
What kind of home worker are you?
#1. Sofa Slumper
You are comfier on the sofa than sat at a table and often find yourself craning over a small screen. Hours can pass as you slide further down the sofa and although you might feel zen, your back is crying out for a posture reset. What’s more, after taking a break to go and eat, you’re back on the sofa to watch TV. Will your spine ever be upright?
Dr Jenkins tip: Place a cushion under your bottom and behind your back to correct your posture.
#2. Desk Roller
You are replicating the office environment: a desk, a chair and you’re (hopefully) sat upright. However, it can be tricky to avoid hunching over a laptop screen unless you’re set up with a big at-eye-level monitor. Tense shoulders and posture that slumps as the day goes on can wreak havoc with your poor back.
Dr Jenkins tip: Make sure your screen is at eye level by placing your laptop on a stack of books.
#3. Kitchen Cruncher
A lack of space means standing at your kitchen worktop squeezed in between the blender and kettle. Naturally, a worktop doesn’t offer the comfiest work stations and your spine soon finds itself curled over a keyboard for hours on end. You might even start placing all your weight on one leg, causing an imbalance in your spine.
Dr Jenkins tip: Ensure that both feet are flat on the floor at any given time and that you focus on standing up straight.
#4. The Pacer
Whether through choice, or lack of space, classic traits of a Pacer involve wandering from room to room, carrying the laptop in one arm and often, a phone in the other. It’s a case of working wherever there’s space, even if it’s crossed legged on the floor which has a tendency to put your back into a slumped position.
Dr Jenkins tip: Walking around is better than sitting but make sure you use a couple of cushions when you sit on the floor and try to keep your screen as close as possible to eye level.
Check out www.mindyourbackuk.com for more tips on caring for your back.


