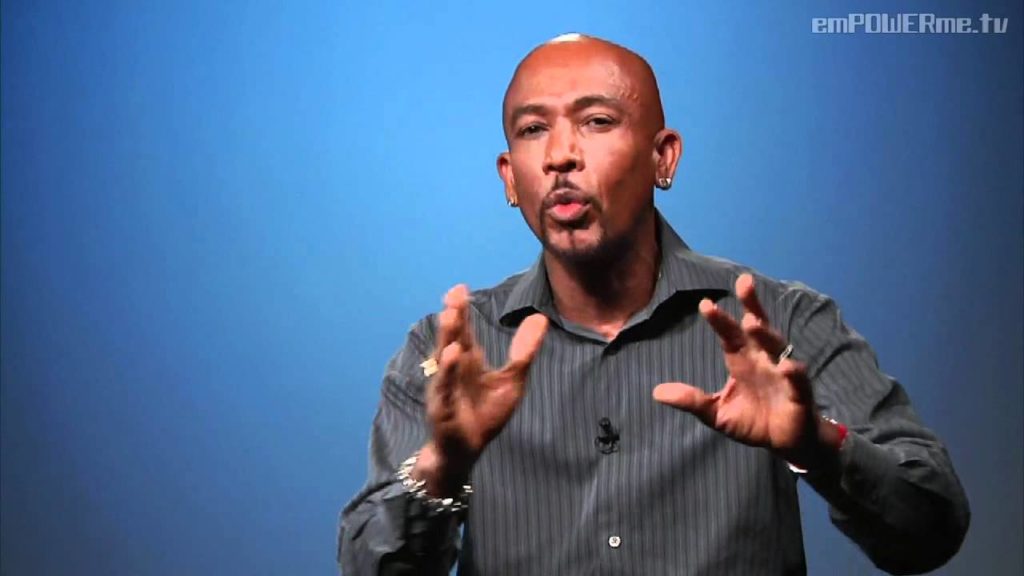
Emmy award winning TV host, Montel Williams, who has been living with multiple sclerosis for nearly 20 years. Montel shares some of the challenges he has had to overcome to lead a healthy and prosperous life living with multiple sclerosis . He gives tips on exercise, diet and his personal juicing recipe!
ms
Multiple sclerosis – ‘I consider myself very lucky’
Sara was 22 when she was diagnosed with relapsing remitting multiple sclerosis (MS).
“It all started when I was in my final year of university. I was travelling home from a job interview when somebody stole my purse. It was very upsetting.
“Then I woke the next day and couldn’t see properly. My vision was blurry in my left eye, and I couldn’t see colours clearly. I also had pain behind my eye. I went to the doctor, thinking it would be something like conjunctivitis, but my GP was so concerned that she sent me to hospital that night.
“After a series of tests I was diagnosed with optic neuritis, which is the swelling of the optic nerve. I didn’t realise it at the time, but this is sometimes one of the first signs of MS.
“I then saw a neurologist and had a magnetic resonance imaging (MRI) scan and some really uncomfortable eye tests. I was diagnosed with relapsing remitting MS and felt very scared.
“By this time, it was six months after my initial eye problems and I was struggling to walk. I was weak, shaky and felt a lot of tingling in my body. My parents noticed I was dragging my left leg. But I think these symptoms were linked to stress – it was just after September 11th, and I remember feeling absolutely devastated.
“I was very fortunate. My neurologist thought I was very well-suited for beta interferon injections. Beta interferon is a disease-modifying medicine that reduces the number and severity of MS relapses.
“Three months later, I was approved for this treatment and started my weekly injections. The side effects were absolutely dreadful. I had flu-like symptoms, which began 24 to 48 hours after the injection.
“I’m still on the injections now, aged 30. Fortunately the side effects have now become less severe, although I do still suffer from them. Because the disease and treatment side effects can make you feel lousy, I’m prone to depression, so I also take antidepressants.
“But by looking at me, you’d never know I have the illness. I work full-time for the NHS, and am doing a Masters degree. I find that it really helps to keep a positive mental attitude.
“I still suffer from fatigue and eye problems, and I now wear glasses. Some days, when my leg isn’t working well, I just take it easy. My work colleagues have been very supportive.
“When I go for my hospital check-ups twice a year, I see people in wheelchairs who are clearly in a much worse condition than I am. I consider myself very lucky.”
Multiple Sclerosis – Diagnosing MS
It can be hard to tell whether your symptoms might be caused by multiple sclerosis (MS) at first, as some of the symptoms can be quite vague or similar to other conditions.
See your GP if you think you have symptoms of MS. Letting them know about the type and pattern of symptoms you’re experiencing in detail will help them determine whether you might have the condition.
If your GP thinks you could have MS, you should see a neurologist (a specialist in conditions of the nervous system) for a specialist assessment.
Tests for MS
Diagnosing MS is complicated because no single test can positively diagnose it. Other possible causes of your symptoms may need to be ruled out first.
It may also not be possible to confirm a diagnosis if you have had only one “attack” of MS-like symptoms. A diagnosis can only be made with confidence once there’s evidence of at least two separate attacks, although this may include signs of attacks on an MRI scan that you may not realise you have had.
Some of the tests you may need to confirm MS are outlined below.
Neurological examination
Your neurologist will look for abnormalities, changes or weakness in your vision, eye movements, hand or leg strength, balance and co-ordination, speech and reflexes.
These may show whether your nerves are damaged in a way that might suggest MS.
Magnetic resonance imaging (MRI) scan
A magnetic resonance imaging (MRI) scan is a painless scan that uses strong magnetic fields and radio waves to produce detailed images of the inside of the body.
It can show whether there’s any damage or scarring of the myelin sheath (the layer surrounding your nerves) in your brain and spinal cord. Finding this can help confirm a diagnosis in most people with MS.
A standard MRI scanner is like a large tube or tunnel. The machine is noisy and some people feel claustrophobic while the scan is done. Tell your neurologist if you’re worried about this.
Newer scanners are more open and work quicker than those used in the past, and most people have scans without any problems.
Evoked potential test
There are several types of evoked potential test.
The most common type assesses how well the eyes work. Light patterns are shown to the eyes while your brainwaves are monitored using small, sticky patches called electrodes placed on your head.
It’s a painless test and can show whether it takes your brain longer than normal to receive messages.
Lumbar puncture
A lumbar puncture is a procedure to remove a sample of your spinal fluid by inserting a needle into the lower back. Spinal fluid is the fluid that surrounds your brain and spinal cord, and changes in the fluid can suggest problems with the nervous system.
The procedure is done under local anaesthetic, which means you’ll be awake, but the area the needle goes in will be numbed. The sample is then tested for immune cells and antibodies, which is a sign that your immune system has been fighting a disease in your brain and spinal cord.
Lumbar punctures are very safe, but are often uncomfortable and can cause a headache that occasionally lasts for up to a few days.
A lumbar puncture will often be performed to provide extra information if your symptoms or scans are unusual.
Blood tests
Blood tests are usually performed to rule out other causes of your symptoms, such as vitamin deficiencies or a very rare, but potentially very similar, condition called neuromyelitis optica.
Determining the type of MS
Once a diagnosis of MS has been made, your neurologist may be able to identify which type of MS you have.
This will largely be based on:
the pattern of your symptoms – such as whether you experience periods when your symptoms get worse (relapses) then improve (remissions), or whether they get steadily worse (progress)
the results of an MRI scan – such as whether there’s evidence that lesions in your nervous system have developed at different times and at different places in your body
However, the type of MS you have often only becomes clear over time because the symptoms of MS are so varied and unpredictable. It can take a few years to make an accurate diagnosis of progressive MS, as the condition usually worsens slowly.
- Brain
- The brain controls thought, memory and emotion. It sends messages to the body controlling movement, speech and senses.
- Inflammation
- Inflammation is the body’s response to infection, irritation or injury, which causes redness, swelling, pain and sometimes a feeling of heat in the affected area.
- Lesions
- A lesion is an abnormal change in an organ or body tissue because of injury or disease.
- MRI
- MRI stands for magnetic resonance imaging. It is the use of magnets and radio waves to take detailed pictures of inside the body.