
Join me as I explore several health conditions that are believed to be more prevalent in the autistic community than in the neurotypical population.
Research suggests that alterations in the gut microbiome before the onset of rheumatoid arthritis may present an opportunity for preventive treatments.
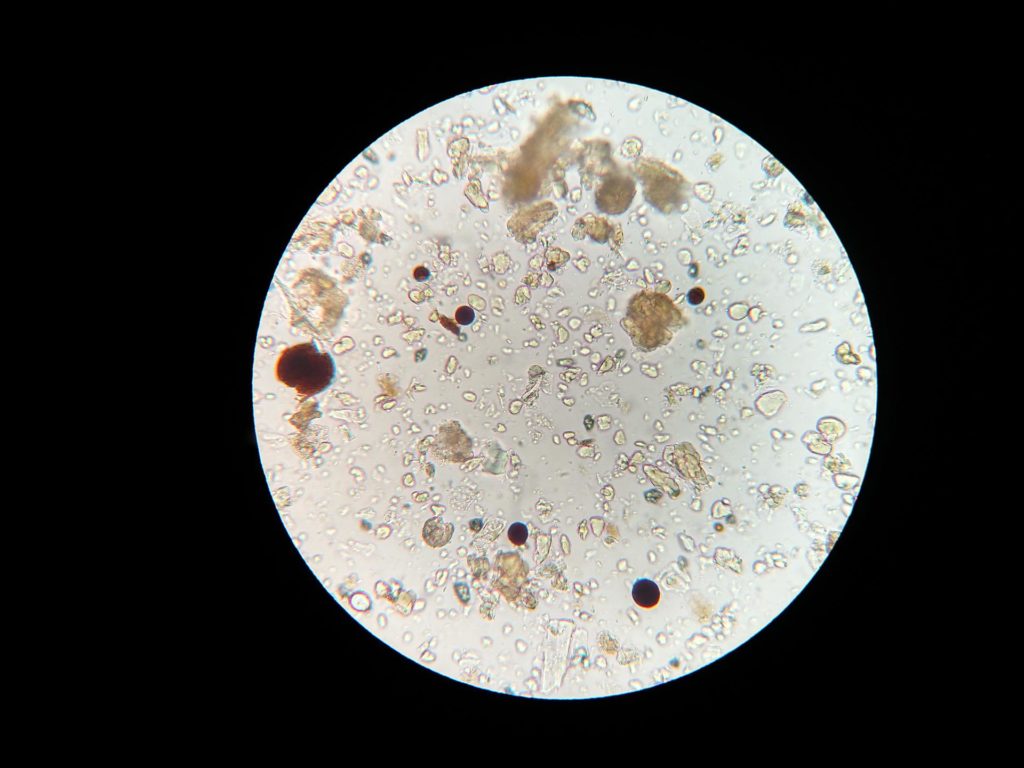
According to a longitudinal study conducted by researchers in Leeds, bacteria linked to inflammation are found in the gut in higher amounts about ten months before patients develop clinical rheumatoid arthritis.
Rheumatoid arthritis, which affects over half a million people in the UK, is a chronic disease that causes swelling, pain, and stiffness in the joints. The immune system mistakenly attacks the body’s healthy cells, causing the disease.
Previous research has connected rheumatoid arthritis to the gut microbiome, the community of microbes in the intestines. However, this recent study, published in the Annals of the Rheumatic Diseases, reveals a potential intervention point.
Lead researcher Dr. Christopher Rooney stated: “Patients at risk for rheumatoid arthritis often experience symptoms like fatigue and joint pain. They may also have a family member who has developed the disease. Since there is currently no cure, at-risk patients frequently feel a sense of hopelessness and may even avoid getting tested.”
“This new research might allow us to act sooner to prevent rheumatoid arthritis.”
Versus Arthritis funded the longitudinal study involving 19 patients at risk of rheumatoid arthritis. Samples were taken five times over 15 months.
Five of these patients progressed to clinical arthritis, and the research showed they had gut instability with higher amounts of bacteria, including Prevotella, which is associated with rheumatoid arthritis, about ten months before progression. The remaining 14, whose disease didn’t progress, had largely stable bacteria in their gut.
Potential treatments that the researchers want to test during the ten-month window include changes to diet, such as eating more fibre, taking prebiotics or probiotics, and improving dental hygiene to keep harmful bacteria from periodontal disease away from the gut.
The exact relationship between gut inflammation and rheumatoid arthritis development remains unclear. In a small number of patients within the study, the gut changes occurred before a rheumatologist observed any joint changes. Still, more research is needed to determine whether these influence each other.
Although bacteria is associated with rheumatoid arthritis, the researchers want to emphasize that there is no evidence that it is contagious.
Lucy Donaldson, director for research and health intelligence at Versus Arthritis, said: “At Versus Arthritis, we welcome the findings of this study, which could give the clinicians of the future a crucial window of opportunity to delay – or even prevent – the onset of rheumatoid arthritis. This success is a testament to UK researchers’ dedication to personalising treatment and preventing chronic conditions that significantly impact a person’s ability to work, raise families and live independently.”
The study initially collected data from 124 individuals with high levels of CCP+, an antibody that attacks healthy cells in the blood and indicates a risk of developing rheumatoid arthritis. The researchers compared their samples to 22 healthy individuals and seven people with a new rheumatoid arthritis diagnosis.
The findings from this larger group showed that the gut microbiome was less diverse in the at-risk group compared to the healthy control group.
The longitudinal study, which took samples from 19 patients over 15 months, revealed the changes in bacteria at ten months before progression to rheumatoid arthritis.
On average, the rates of relapses, accumulation of disability, and even mortality are decreasing in people with multiple sclerosis. This video presents historical and modern studies that demonstrate this clear trend. But what is causing this improvement? Is it due to better diagnoses, changes in diagnostic criteria, or the effectiveness of disease-modifying therapies?