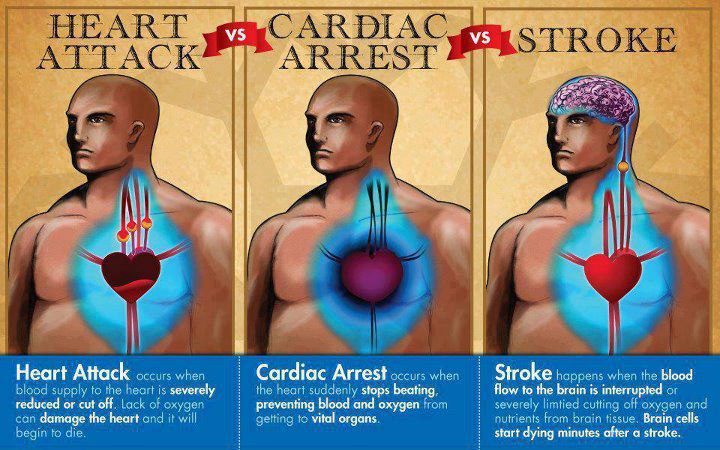
A study of more than 100,000 people with type 2 diabetes (T2D), presented at the annual meeting of the European Association for the Study of Diabetes (EASD), held online this year, found that insulin resistance is associated with stroke.
The higher the insulin resistance, the greater the risk of stroke, the research, from Dr Alexander Zabala and colleagues at the Karolinska Institute and researchers at Gothenburg University and the National Diabetes Registry in Sweden, found.
Insulin resistance – when the body’s cells don’t respond properly to insulin and can’t easily take up glucose from blood – is a key feature of T2D and levels vary from patient to patient.
Dr Zabala used estimated glucose disposal rate (eGDR) as a measure of insulin resistance.
eGDR has previously been shown to be a good proxy for insulin resistance and is calculated using a formula that factors in a patient’s waist circumference, HbA1c (average blood sugar level) and whether they have high blood pressure.
Health records were used to calculate the eGDR of 104,697 T2D patients in Sweden. The participants had an average age of 63 and 44.5% were female.
They were followed up for an average of 5.6 years, during which 4,201 (4%) had a stroke.
Analysis revealed that the higher a person’s insulin resistance, the greater their chance of having a stroke. Those with the lowest insulin resistance (the highest eGDR) were 40% less likely to have a stroke than those with the highest insulin resistance.
Age, cholesterol levels, smoking, heart conditions and other traditional risk factors for stroke were all adjusted for.
The study also found that higher insulin resistance was linked to a higher risk of death after a stroke. Those with the lowest resistance were 28 per less likely to die during the follow-up period than those with the most severe insulin resistance.
Further analysis showed high blood pressure to be more strongly linked to stroke than waist circumference or HbA1c.
The study’s authors conclude: “We found that in individuals with type 2 diabetes, a low eGDR, a simple measure of insulin resistance, was associated with an increased risk of stroke and mortality.”
Dr Zabala adds: “eGDR could be used to help T2D patients better understand and manage their risk of stroke and death.
“It could also be of importance in research. In this era of personalised medicine, better stratification of type 2 diabetes patients will help optimise clinical trials and further vital research into treatment, diagnosis, care and prevention.”