Atrial l Fib
The NHS regulator NICE has today recommended that people taking a thinning agent can monitor their own blood levels at a time and place convenient to them. In the guidance, NICE recommends using the CoaguChek® XS self-monitoring device.
This means that more people taking a thinning agent should be able to self-monitor (or ‘SelfieChek’), rather than being tied to frequent (sometimes weekly) clinic or hospital visits to have their blood clotting levels measured. Self-monitoring allows people taking a thinning agent to enjoy a flexible lifestyle and reduces the risk of stroke for people with atrial fibrillation or a replacement heart valve.The guidance is also set to benefit the NHS by reducing the unnecessary burden that regular blood checks place on healthcare professionals’ time and resources.
PatientTalk.Org spoke to Eve Knight of Anticoagulation Europe, about the background and implications of the new regulations. Cody conducted the interview on our behalf.
CODY– If you could just start by telling us a little bit about yourself, who you are, and what you do and what your role is?
EVE KNIGHT My name is Eve Knight and I’m co-founder and chief executive of the charity of the Anticoagulation Europe, chief executive basically means I’m responsible for everything although I do have a really great team who work with me and lots and lots of volunteers around the country.
CODY So what’s the cause of the Anticoagulation Europe, what are you guys trying to achieve?
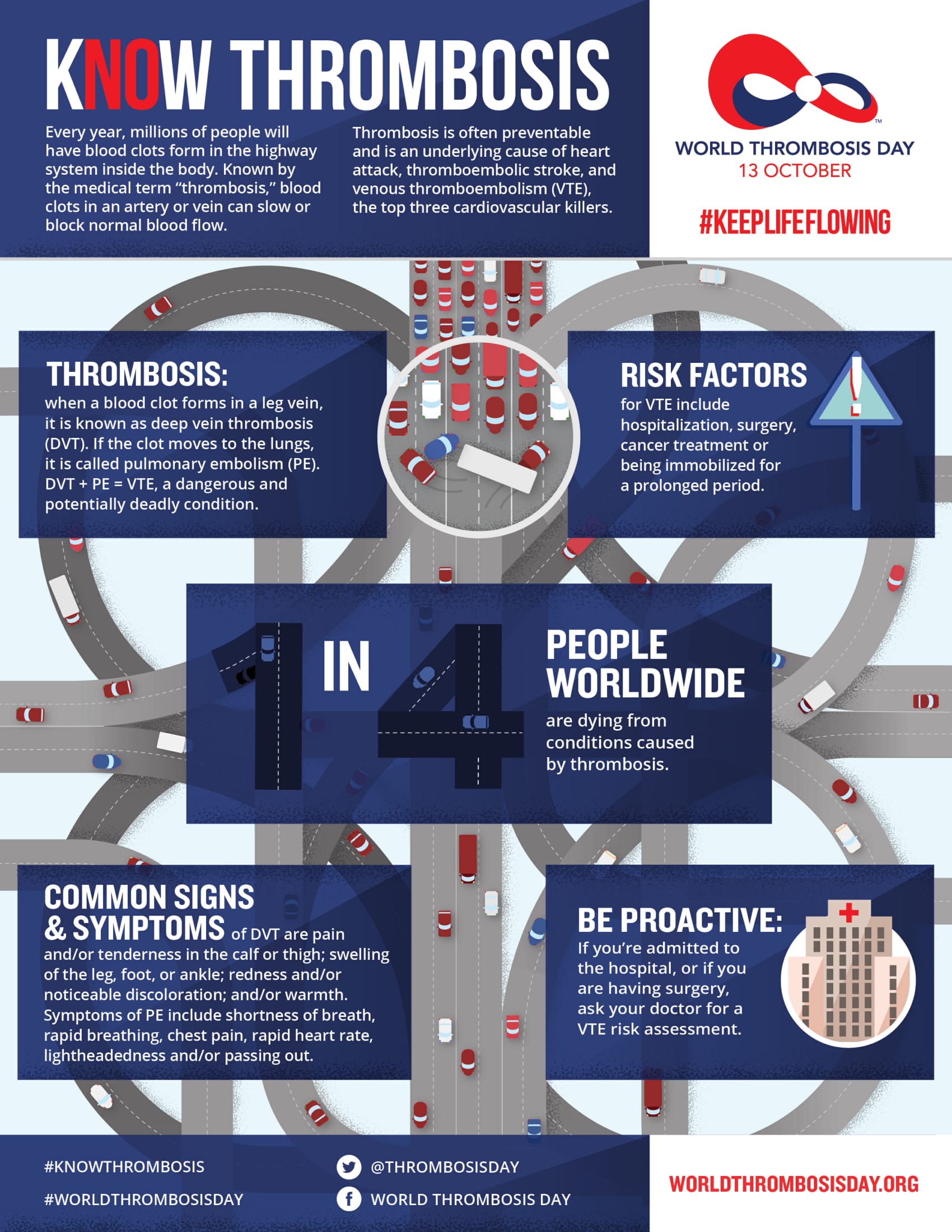
EVE KNIGHT Anticoagulation Europe was founded 14 years ago, our aims are the prevention of thrombosis, the provision of information and support for health care professional and patients and their families and to make sure that the patient voice is at the centre of everything of the NHS does, particularly anyone who is designing anticoagulation services.
CODY Great, so were talking today about Atrial Fibrillation and some new NICE guidelines, so could you just explain to us why anyone would need to take a blood thinning agent? So what conditions require it and how does it work?
EVE KNIGHT There are a number of conditions that you would need to take an thinning agent, Atrial Fibrillation being one of them, replacements heart valves, deep vein thrombosis, Pulmonary embolism and genetic clotting conditions, the guidance that has been issued today is specifically for Atrial Fibrillation and replacement heart valves.
CODY So how does the blood thinning work?
EVE KNIGHT It doesn’t actually thin the blood, what warfarin does is to inhibit the production of Vitamin K in your liver, vitamin K is the vitamin that causes your blood to clot and we all need our blood to clot otherwise when we cut ourselves we would bleed to death. Warfarin inhibits the production so not so much Vitamin K is produced so your blood takes longer to clot.
CODY So who does Atrial Fibrillation affect because I was reading through this today and I was surprised to find out that it actually affects quite a few young people as well as old?
EVE KNIGHT It does affect young people , the major co halt of patients are older, 1 in 8 of us by the time we are 65 will have Atrial Fibrillation but it does affect younger people and what your trying to do with warfarin is to reduce the risks of strokes and young people regrettable do have strokes.
CODY Do you have any idea how many people this condition affects and how many people are treated with a thinning agent at the moment?
EVE KNIGHT In the UK about 1 million and a quarter of people are on warfarin, there’s about 800,000 people diagnosed with Atrial Fibrillation and approximately 40% of those are not on an Anticoagulant or they may be on aspirin and aspirin Nice have now said is no good for preventing strokes you have to be on an Anticoagulant, So there’s a huge co halt of patients who will now need to go onto an Anticoagulant.
CODY – And that was during this year?
EVE KNIGHT That was in June this year yes.
CODY – Do you know why they decided to make that recommendation?
EVE KNIGHT – Well this was a complete update of their 2006 guidance and they made several new points, it’s long been thought or known that aspirin is not as effective as warfarin as preventing strokes and yet it carries virtually the same bleeding risks. So finally the sway of opinion has come together on that and NICE have said that aspirin no longer be used as a mono therapy in preventing strokes for AF.
CODY – So someone on this kind of treatment, how often do they have to visit a clinic or a hospital for check-ups?
EVE KNIGHT That depends very much, everybody on thinning agent will be given a therapeutic range and that will differ depending on the condition for which you’re taking it. In the first few weeks when you go onto a thinning agent you are very likely to be very unstable so you may be going every 3 days/ twice a week, it will for most people eventually settle down and then for a lot of people it varies between once a week and once every six weeks.
CODY – So even when it settles down it’s a lot of visits?
EVE KNIGHT – It’s a lot of visits and it does very much depend, you know a thinning agent is quite an unstable product with a very narrow therapeutic window. So things you would normally do, things you would eat, things you drink, other things you take, all of these can have an effect on a thinning agent and make it go up or down and that would mean you go out of your range and if you go too high out of your range you’re at risk of a bleed and too low out of your range you at the risk of a clot and if your dose, if your range is varying, then you dose will need to be altered.
CODY – Can you briefly just explain the role that NICE plays? Who they are to be issuing recommendations?
EVE KNIGHT NICE is the body that issues recommendations and regulations for what is used drugs or diagnostic tools within the NHS.
CODY So they have recommended that people can now monitor their blood levels at home. Can you explain a little bit about how the CoaguChek device works?
EVE KNIGHT NICE have recommended for people with AF and replacement heart valves that self-monitoring is clinically effective, it’s safe and it’s cost effective for the NHS. A CoaguChek XS is a hand held monitor that you place a little strip into. You prick your finger with a pen needle much the same as diabetics and you take the tiniest drop of blood and you drop that or swipe onto the strip. Within two minutes the monitor gives you your INR range. So it tells you if you’re within your therapeutic range.
CODY Is this quite new technology or is this recommendation coming in after it’s been proven over a period of time?
EVE KNIGHT This recommendation is coming a long time after the technology. In Europe it’s probably 28, 30 years. In this country it’s in excess of 20 years so it’s taken a long time to get to this point but we very much welcome NICE’s recommendation.
CODY Why do you think it’s taken so long for the recommendation to be made if it would seem to be obvious?
EVE KNIGHT To be honest I really don’t know why it’s taken so long. None of the companies have put into NICE for them to look at it. In fact NICE were actually asked by a patient to look at this and I believe that it’s the first time a patient has asked NICE to actually look at something and issue guidance.
CODY That’s interesting. In the same vein why do you think only 15% of GP’s in the UK currently offer self-monitoring to their patients?
EVE KNIGHT I think there are many reasons for that. Cost or the thought that it will cost too much is possibly one. I think a number of GP’s have not been convinced of its safety and now this guidance is out I am hoping that will change that. I think also we tend to take a longer time in this country to actually adopt new technology. I mean the Prime Minister David Cameron actually said in a speech in 2011, he used self-monitoring as an example of what was good about the NHS and what could be used in the NHS but he also recognised in that speech that we are not very good at bringing these things to the table and getting on with them. Now we’ve got the guidance I sincerely hope it’s about time we will get on with it.
CODY So you did mention cost briefly there. I suppose we have to treat it over a long time frame because if you are continuously visiting a GP there is a large cost involved in that as well. What sort of cost outlay is there for this sort of self-checking treatment?
EVE KNIGHT Well there are two sets of costs. Costs for the NHS which is the cost of taking the blood sample, sending it off to the lab, getting it back from the lab, contacting the patient and all that sort of thing. There’s also the cost of if you get it wrong; the cost of strokes. Strokes are extremely expensive things to treat in the NHS. For patients if they are going to clinics or their GP they have got the cost of getting there, the cost of taking time off work/ off school so there are lots of different costs involved. The long term cost savings for the NHS will be two fold. It will be that patients are self-monitoring at home frees up more time for the clinics to deal with people who don’t want too or for people it’s not clinically suitable. Also it has been proven in research that there are less strokes, less thrombotic events when people do self-monitor so the long term costs of saving life’s and saving money is there.
CODY I suppose you can avoid missed appointments and things like that?
EVE KNIGHT You avoid missed appointments and also when you self-monitor because you tend to self-monitor a little more frequently you don’t tend to make so many alterations to your dose so there are less chances of you being in and out of your range.
CODY Anticoagulation Europe are supporting and calling for more self-monitoring. What does success look like for you? 100% uptake?
EVE KNIGHT No there will never be 100% uptake. Some people will not want to self-monitor and that is quite right. No one is saying people have to self-monitor. It is a choice for patients and that’s the beauty of it. Its having a choice about what you want to do and how you want to live your life. Success for me would be getting an awareness of this out to patients and the general public so if they want to they can have these types of conversations with their GP or their anti coag nurse and then make a decision on the benefits of self-monitoring, would it be right for them. Success would also be and we will be campaigning for it, to get these monitors available on prescriptions alongside the strips that go with them so that people are not discriminated against by not being able to afford to purchase this monitoring equipment.