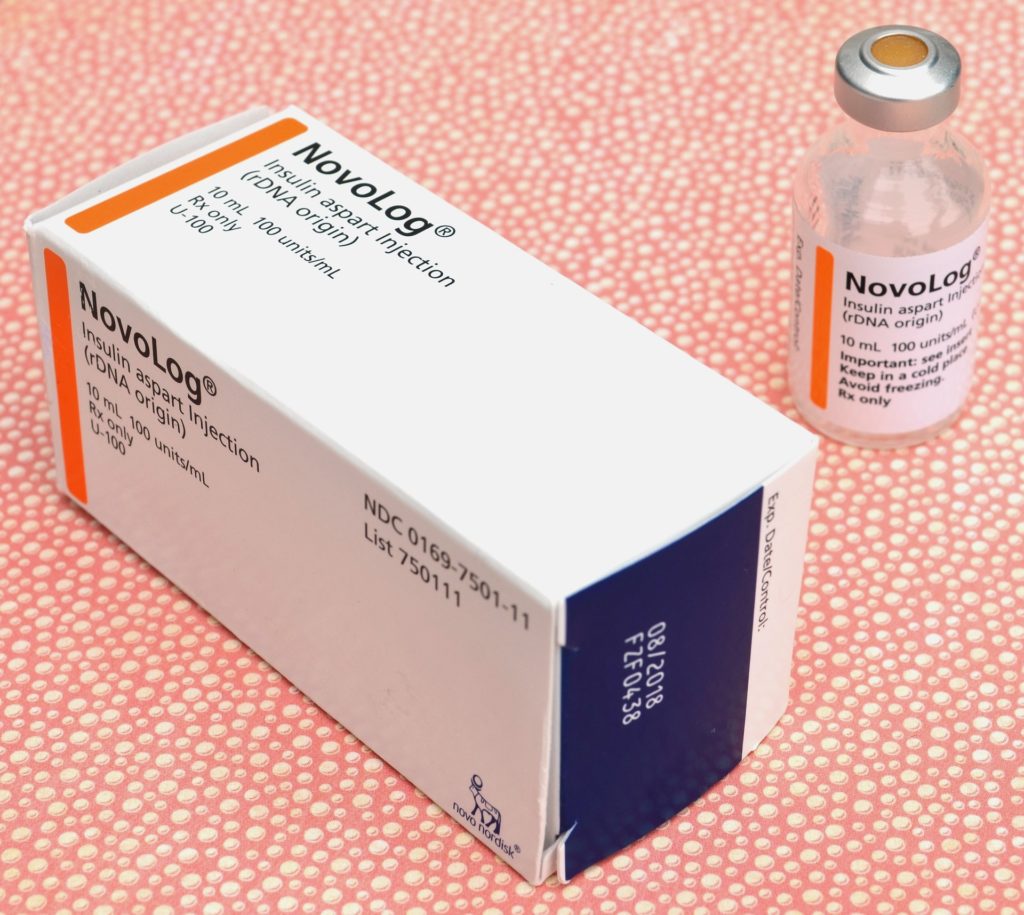
Researchers highlight how manufacturers have listed an increasing number of patents on insulin products over the years. CREDIT Towfiqu barbhuiya, Unsplash (CC0, https://creativecommons.org/publicdomain/zero/1.0/)
Over the last four decades, insulin manufacturers have extended their periods of market exclusivity on brand-name insulin products by employing several strategies, including filing additional patents on their products after FDA approval and obtaining many patents on delivery devices for their insulin products. That is the conclusion of a new analysis of FDA and patent records carried out by William Feldman of Brigham and Women’s Hospital, USA, and colleagues, and published November 16th in the open access journal PLOS Medicine.
Insulin is the primary, life-saving treatment for type 1 and some type 2 diabetes but remains costly in the US even though it was discovered more than a century ago. A 2021 Congressional report found that for decades, the three major manufacturers of insulin continuously raised prices, often in tandem with one another. These high prices are additionally sustained by patents and regulatory exclusivity that limit competition on brand-name products. Patents are government-granted monopolies that last 20 years and the Food and Drug Administration (FDA) cannot approve generic versions of drugs for marketing until patents have expired.
In the new study, researchers used publicly available U.S. FDA and patent data to track all insulin products approved in the U.S. from 1986 to 2019. During the study period, the FDA approved 56 brand-name insulin products.
The researchers found that protection on insulin was enhanced by patents obtained after FDA approval, which lengthened expected market exclusivity by a median of 6 years. Moreover, many patents were on the insulin delivery devices rather than the drugs themselves. In two-thirds of drug-device combinations, the device patents were the last to expire; these last-to-expire device patents extended protection for a median of 5.2 years. Overall, manufacturers secured a median of 16 years of protection on their insulin products through patents and exclusivities, surpassing the median of 14 years observed in other studies of top-selling small-molecule drugs. The insulin lines with the longest periods of expected protection from the first product approved to last-to-expire patent was Lantus (32.9 years), followed by Novolog (32.3 years) and Novolog 70/30 (30.9 years).
“Policy reforms are needed to promote timely competition in the pharmaceutical market and ensure that patients have timely access to drugs at fair prices,” the authors say.
Feldman adds, “Our study highlights how manufacturers have listed an increasing number of patents on insulin products over the years. These patents can delay competition and keep prices high for patients.”