The test was developed using an existing diagnostic procedure as its basis and has the potential to be applied in clinical trials that target the Epstein Barr Virus
A team of research scientists at Trinity College Dublin have developed a new and unique blood test to measure the immune response to the Epstein Barr Virus (EBV) which is the leading risk factor for developing multiple sclerosis (MS). Their findings are published in the journal Neurology Neuroimmunology and Neuroinflammation and have implications for future basic research in further understanding the biology of EBV in MS, but also has the potential to be applied in clinical trials that target the virus.
MS is a chronic neurological disease with no known cure. It affects approximately three million people worldwide and is the second leading cause of disability in young adults. There is a pressing need for better treatments.
A range of viruses relating to MS have been studied in the past but none have had such compelling evidence as EBV. The question the team considered was why do some people have known MS have a rogue immune response to EBV, a common viral infection that is generally asymptomatic?
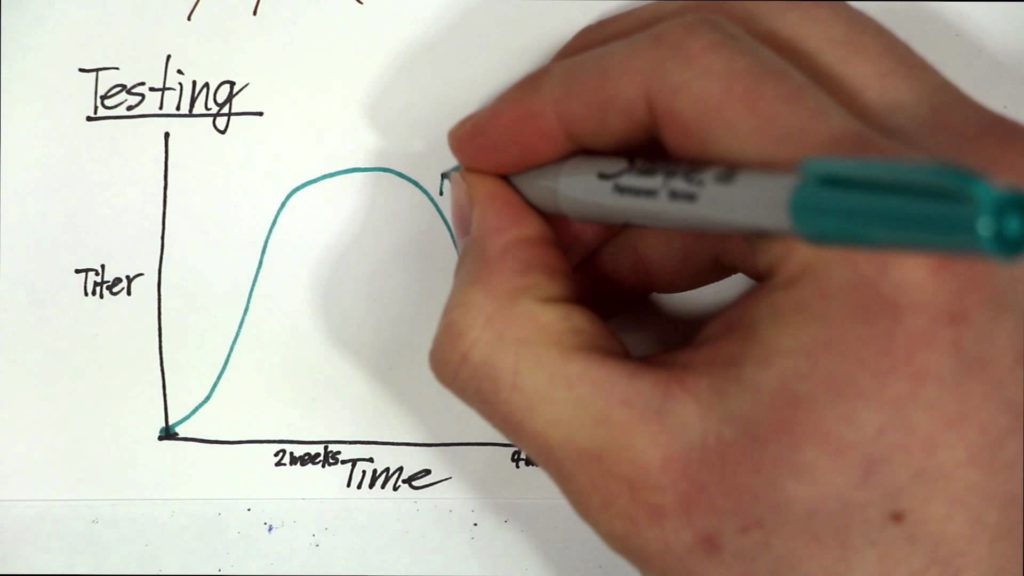
To answer this, scientists measured the cellular response of MS patients to EBNA-1, a part of the EBV that can mimic the myelin coating of nerves which are the principal site of attack of the immune system in MS. The team found that the immune response is higher to EBNA-1 in people with MS compared to those with epilepsy, or the healthy control group. The team also showed that this cellular response is impacted by currently approved medications for MS which target the immune system, but not the virus. The immune response to EBNA-1 was found to be lower in people who are taking B cell depleting medications compared to people with MS not taking medication and the level recorded was equivalent to healthy controls.
B cell depleting medications are effective for reducing MS disease activity. It is not known however, how exactly they work. Many people believe that reducing B cells reduces EBV levels, as EBV can lie dormant within B cells. The scientists do not prove this theory, but do show that the immune response to EBV in MS is equal to healthy controls when these medications are used. The team believe that this supports the need for more selective reduction in EBV rather than targeting all B cells. This is of importance as B cells play an important role in fighting infection and an unselective approach can lead to unwanted side effects.
The Trinity researchers are the first team of scientists to capture the immune response to EBNA-1 using whole blood samples carried out exclusively with equipment that is used in the hospital laboratory day to day. This builds on previous research that used extensive pre-processing in research laboratories. We believe this is of importance as it shows the ability for the test to be run elsewhere and at scale without a need for new equipment or personnel.
This research is important because a standard blood test that was processed in a hospital laboratory provides important information on the immune system’s response to EBNA-1. This response appears to be at the heart of the pathogenesis of MS. The ability to measure this in a scalable test, that was developed using an existing diagnostic test as its basis, has implications for future basic research in further understanding the biology of EBV in MS. But the test also has the potential to be applied in clinical trials that target the virus. This would mean that there is the potential to directly measure the immune response to any potential antiviral treatments, rather than measuring MS outcome measures alone.
Speaking on the potential benefits of this research, Dr Hugh Kearney, Neurologist, School of Medicine, Trinity College and lead author said:
“In the short term the benefit of this research is likely to be for the research community in MS. We believe the approach adopted in this test that uses whole blood samples on a robust hospital-based platform will facilitate adoption in other centres and also replication of the results with a view towards validation. In the medium term, if validated, then this would be of benefit to researchers involved in clinical trials in MS. Long term benefits will be for people with MS, who live with a chronic neurological illness as new treatments tested in clinical trials have the potential to reduce the burden of this potentially disabling disease.
The next step for our team is to develop a longitudinal study. We aim to do this by recruiting newly diagnosed people with MS and measuring this blood test before treatment has started and then repeating the blood test at an interval to show that B cell depletion directly impacts on the cellular response to EBNA-1 in MS.”