Introduction
Actinomycosis is a rare type of bacterial infection caused by a group of bacteria called actinomycetaceae.
Most bacterial infections are confined to one part of the body because the bacteria are unable to penetrate the body’s tissue.
However, actinomycosis is unusual in that the infection is able to move slowly but steadily through body tissue.
Symptoms of actinomycosis vary depending on the type of infection, but can include:
- swelling and inflammation of affected tissue
- tissue damage that results in scar tissue
- formation of abscesses (pus-filled swellings)
- small holes or tunnels that develop in tissue and leak a type of lumpy pus
Read more about the symptoms of actinomycosis.
Types of actinomycosis
In theory, actinomycosis can develop almost anywhere inside the tissue of the human body. But the condition tends to affect certain areas of the body and can be classified into four main types.
They are:
- oral cervicofacial actinomycosis
- thoracic actinomycosis
- abdominal actinomycosis
- pelvic actinomycosis
These are described below.
Oral cervicofacial actinomycosis
Oral cervicofacial actinomycosis is where the infection develops inside the neck, jaw or mouth. In the past, if the condition developed in the jaw it was known as lumpy jaw.
Most cases of oral cervicofacial actinomycosis are caused by dental problems, such as tooth decay or a jaw injury.
Oral cervicofacial actinomycosis is the most common type of actinomycosis, accounting for 50-70% of all cases.
Thoracic actinomycosis
Thoracic actinomycosis is where the infection develops inside the lungs or associated airways.
Most cases of thoracic actinomycosis are thought to be caused by people accidentally inhaling droplets of contaminated fluid into their lungs.
Thoracic actinomycosis accounts for an estimated 15-20% of cases.
Abdominal actinomycosis
Abdominal actinomycosis is where the infection develops inside the abdomen (tummy).
This type of actinomycosis can have a range of potential causes. It can develop as a secondary complication of a more common infection, such as appendicitis, or after accidentally swallowing a foreign object, such as a chicken bone.
Abdominal actinomycosis accounts for an estimated 20% of all cases.
Pelvic actinomycosis
Pelvic actinomycosis is where the infection develops inside the pelvis.
It usually only occurs in women because most cases are caused when the actinomyces bacteria are spread from the female genitals into the pelvis.
Most cases of pelvic actinomycosis are thought to be associated with the long-term use of an intrauterine device (IUD). This type of contraceptive is often known as the coil.
Pelvic actinomycosis usually only occurs if the coil is left in for longer than the manufacturer recommends.
Pelvic actinomycosis accounts for an estimated 10% of all cases.
What causes actinomycosis?
Actinomycosis is caused by a family of bacteria known as actinomycetaceae. In most cases, the bacteria live harmlessly on the lining of the mouth, throat, digestive system and vagina (in women).
The bacteria only pose a problem if the tissue lining becomes damaged by injury or disease, allowing the bacteria to penetrate deeper into the body.
This is potentially serious because these are anaerobic bacteria, which means they thrive in parts of the body where there isn’t much oxygen, such as deep inside body tissues.
However, an advantage of actinomyces bacteria being anaerobic is that they can’t survive outside the human body. This means that actinomycosis isn’t a contagious condition.
Read more about the causes of actinomycosis.
Diagnosing actinomycosis
In its initial stages, actinomycosis can be a challenging condition to diagnose correctly because it shares symptoms with other more common conditions. It’s often only discovered during tests or surgery to check for other conditions.
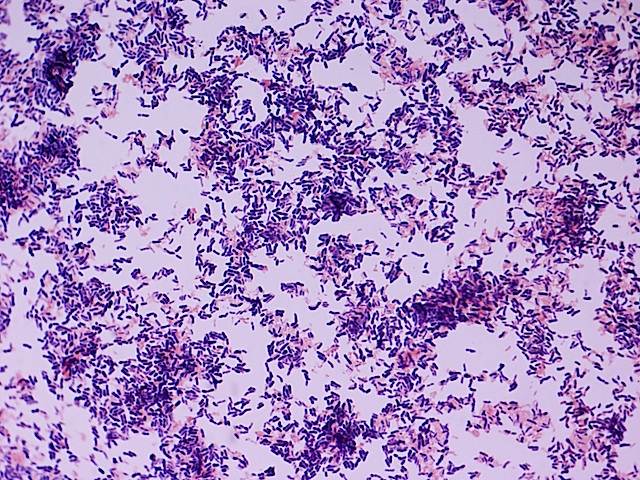
For example, many cases of actinomycosis are detected when biopsies are carried out to check for cancer. A biopsy is where a small tissue sample is removed so it can be examined under a microscope.
Actinomycosis can usually be more confidently diagnosed in its later stages, after the sinus tracts have appeared in the surface of the skin.
This is because the sulphur granules produced by the sinus tracts during an actinomycosis infection have a distinctive shape that can be identified under a microscope.
Treating actinomycosis
Actinomycosis usually responds well to treatment, which involves taking a long-term course of antibiotics.
Antibiotics
An initial course of antibiotic injections is usually recommended for 2 to 6 weeks, followed by antibiotic tablets for another 6 to 12 months.
A nurse should be able to teach you how to administer antibiotic injections at home so you don’t need to stay in hospital for the duration of the course.
The preferred antibiotics for treating actinomycosis are benzylpenicillin, which is used for the antibiotic injections, and amoxicillin tablets.
In some cases, other bacteria are also present and more than one antibiotic or other antibiotics will need to be given.
Side effects of these antibiotics include:
- diarrhoea
- nausea (feeling sick)
- skin rash
- increased vulnerability to fungal infections, such as oral thrush (a fungal infection that occurs in the mouth)
If you’re allergic to penicillin, alternative antibiotics such as tetracycline or erythromycin can be used.
Read more about antibiotics.
Surgery
In some cases, minor surgery may be required to repair the damaged tissue and drain pus out of the abscesses.
Complications of actinomycosis
Abscesses that develop as a result of actinomycosis may form in many parts of your body, including your lungs. They can spread easily from one part of your body to another.
If the original site of the infection is located in the skin of your face, it may spread to nearby parts of your body, such as your scalp or ears.
If the original site of the infection is your mouth, it may spread to your tongue, larynx (voicebox), trachea (windpipe) and salivary glands, and the tubes that connect your throat to your nose.
If the infection spreads to your brain, a brain abscess could develop.
Preventing actinomycosis
Most cases of oral actinomycosis occur as a result of poor dental hygiene. This means practising good dental hygiene is the best way to prevent actinomycosis.
Read about preventing tooth decay and dental health for more information and advice about good oral hygiene practices.