Acne is a common skin condition that affects most people at some point. It causes spots to develop on the skin, usually on the face, back and chest.

Acne?
The spots can range from surface blackheads and whiteheads – which are often mild – to deep, inflamed, pus-filled pustules and cysts, which can be severe and long-lasting and lead to scarring.
Read more about the symptoms of acne.
What can I do if I have acne?
Keeping your skin clean is important, but will not prevent new spots developing. Wash the affected area twice a day with a mild soap or cleanser, but do not scrub the skin too hard to avoid irritating it.
If your skin is dry, use a moisturiser . Most of these are now tested so they don’t cause spots (non-comedogenic).
Although acne can’t be cured, it can be controlled with treatment. Several creams, lotions and gels for treating spots are available at pharmacies.
If you develop acne, it’s a good idea to speak to your pharmacist for advice. Products containing a low concentration of benzoyl peroxide may be recommended, but be careful as this can bleach clothing.
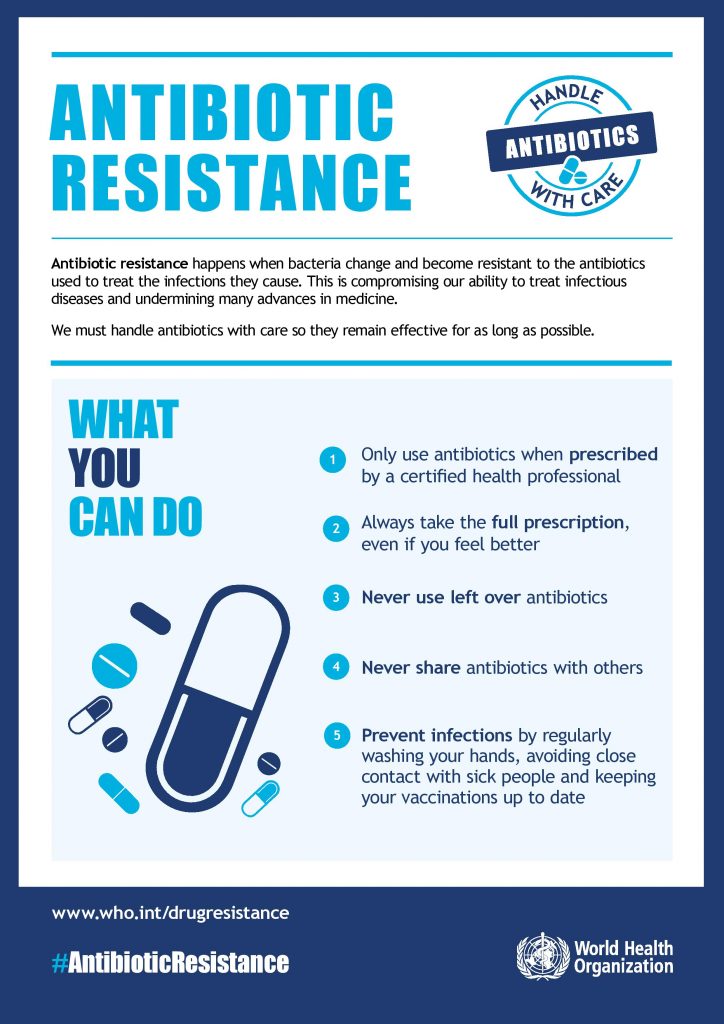
If your acne is severe or appears on your chest and back, it may need to be treated with antibiotics or stronger creams that are only available on prescription.
When to see your GP
See your GP if you cannot control your acne with over-the-counter medication or if it is causing you distress and making you feel unhappy.
Also see your GP if you develop nodules or cysts, as they will need to be treated properly to avoid scarring.
Treatments can take up to three months to work, so don’t expect results overnight. Once they do start to work, the results are usually good.
Read more about treating acne.
Try to resist the temptation to pick or squeeze the spots as this can lead to permanent scarring.
Find out more about complications of acne.
Why do I have acne?

Ehlers-Danlos syndrome.
Acne is most commonly linked to the changes in hormone levels during puberty, but can start at any age.
It affects the grease-producing glands next to the hair follicles in the skin. Certain hormones cause these glands to produce larger amounts of oil (abnormal sebum).
This abnormal sebum changes the activity of a usually harmless skin bacterium called P. acnes, which becomes more aggressive and causes inflammation and pus.
The hormones also thicken the inner lining of the hair follicle, causing blockage of the pores (opening of the hair follicles). Cleaning the skin does not help remove this blockage.
Acne is known to run in families. If both your mother and father had acne, it is likely that you will also have acne.
Hormonal changes, such as those that occur during the menstrual cycle or pregnancy, can also lead to episodes of acne in women.
There is no evidence that diet, poor hygiene or sexual activity play a role in acne.
Read more about the causes of acne, including some common acne myths.
Who is affected?
Acne is very common in teenagers and younger adults. About 80% of people between the ages of 11 and 30 will be affected by acne.
Acne is most common between the ages of 14 and 17 in girls, and boys between 16 and 19.
Most people have acne on and off for several years before their symptoms start to improve as they get older. Acne often disappears when a person is in their mid-twenties.
In some cases, acne can continue into adult life. About 5% of women and 1% of men have acne over the age of 25.
Despite being one of the most widespread skin conditions, acne is also one of the most poorly understood. There are many myths and misconceptions about it: