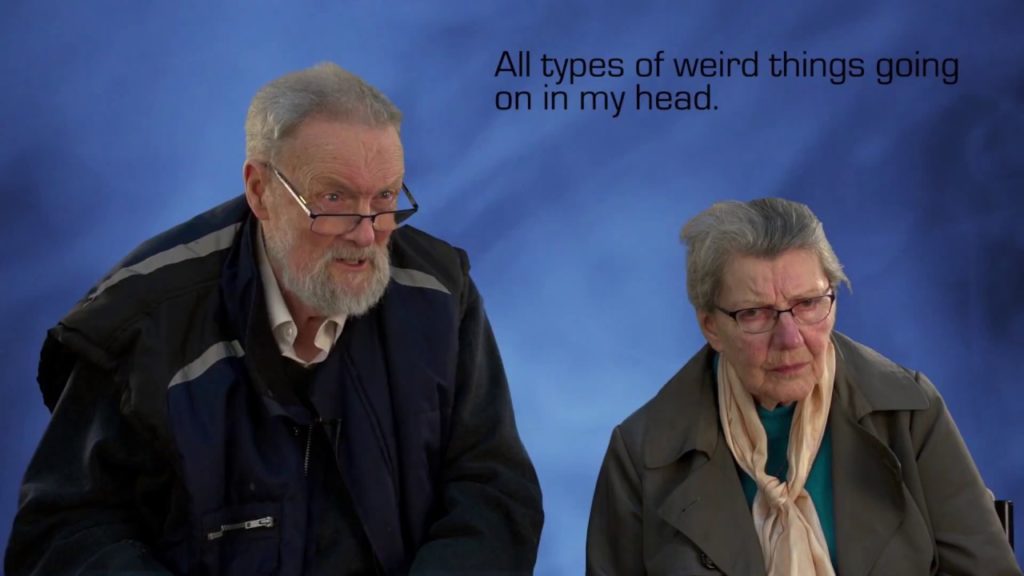
This is David and his wife Gloria’s story. Two years ago David was treated at Leicester’s Hospitals for community acquired pneumonia. During his admission David experienced an episode of delirium. Patients with delirium frequently experience hallucinations, false ideas or paranoia. These symptoms can be very distressing and frightening for patients and their families.
David explains what the experience was like: “Slowly but surely I descended into this land of…well it was different. Unfortunately my brain was telling me this isn’t real but no matter what I did I couldn’t wake up, I couldn’t get rid of it. This is the first experience, it was quite frightening.”
Patients may act in a way that is not normal for them, leading them to be labelled a nuisance or troublesome. David was isolated due to his ‘rude’ behaviour, which was very out of character. David adds: “All types of weird things were going on in my head. The whole thing was quite terrifying but I remember speaking to Gloria on the phone to tell her there was a bomb going to go off. I was firmly convinced this was going to happen. This thought was there but I knew it was wrong.”
It is important to recognise this is not the patient’s fault, in this case David, and to help re-orientate them to their surroundings and the care that they are being provided with.
Delirium can also have a significant impact on family and carers. Gloria didn’t know how to respond: “I didn’t know whether to say you’ll be ok it’s not really happening or to say thank you for the last 64 years, it’s been nice knowing you… you just don’t know how to reply to a person. I found it very difficult. Delirium can change the character of a person; this can be very distressing and difficult to understand for loved ones. A better understanding can help lessen the distress and family members can work alongside healthcare professionals to resolve the delirium quicker.”
Slowly but surely reality returned for David, who says: “Two years later it is still clear in my head what I was thinking. It is quote frightening. It felt so real. You can taste it. The only regret I have is that I would like to go back to say sorry to those people, if they all existed and I didn’t make them up, that I was rude to.”
Dr Chris Miller, Geriatric Medicine Specialist Doctor at Leicester’s Hospitals, looks after patients like David: “Delirium affects up to half our adult inpatients. Those with chronic conditions such as dementia, or Parkinson’s disease, and those with sensory deficits such as visual or hearing impairments are more at risk. Unfortunately, delirium is not very well recognised and frequently leads to poorer outcomes. Patients are often distressed by these episodes. A lack of understanding of this medical condition can exacerbate problems.”
David spent three weeks in hospital recovering from his pneumonia and delirium. He was subsequently discharged home to his wife, Gloria. He remains distressed by his experiences of delirium that he still remembers vividly.
As Chris highlights: “We encourage our staff to ask if their patients are more confused or more withdrawn than normal and if so, to ‘THINK DELIRIUM’ and work to find, investigate and treat any cause. Similarly, if family members or carers notice their loved one is more confused or more withdrawn than their normal self to alert our staff to this. Prompt actions can reduce the severity of any episode and improve outcomes for our patients.”
We would like to thank David and Gloria for sharing their story.